Pyoderma gangrenosum is a rare and often misunderstood skin condition that can have a significant impact on a person’s quality of life. This painful and progressive disorder causes deep ulcers, typically on the legs, which can spread rapidly and be difficult to treat. Despite its name, pyoderma gangrenosum is not caused by infection or gangrene, but is believed to be an autoimmune disorder with complex underlying mechanisms.
Understanding pyoderma gangrenosum is crucial for both healthcare providers and patients to ensure timely diagnosis and effective management. This article delves into the key aspects of this challenging condition, including its clinical presentation, diagnostic criteria, and comprehensive treatment approaches. It also explores the long-term outlook for individuals living with pyoderma gangrenosum and highlights the importance of a multidisciplinary care team in managing this chronic skin disorder.
Clinical Presentation of Pyoderma Gangrenosum
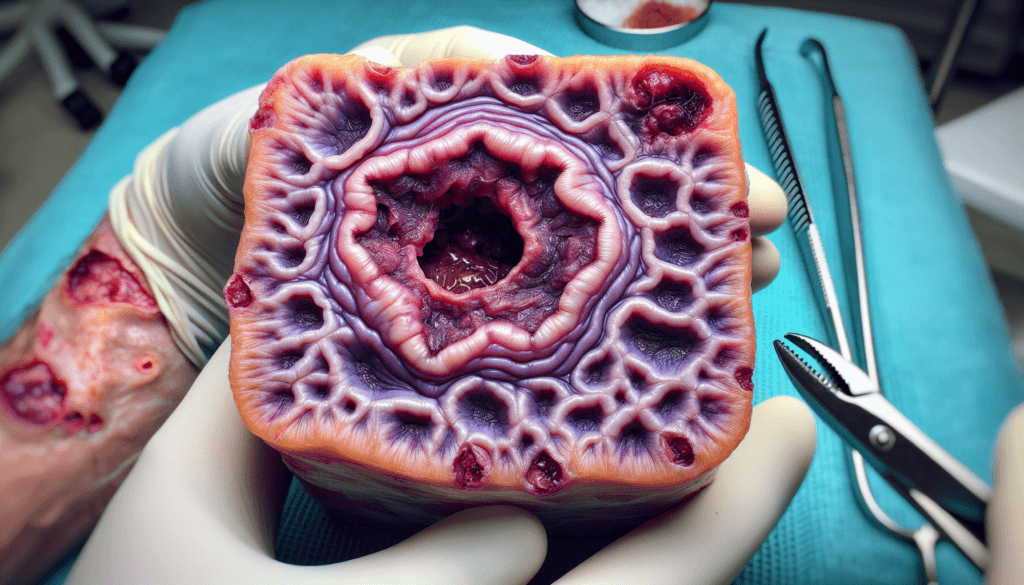
Pyoderma gangrenosum typically presents as an extremely painful, rapidly progressing ulcer with a violaceous, undermined border. The lesion often starts as a tender papule, pustule, or bulla that quickly erodes to form an ulcer. The ulcer can deepen and expand rapidly, causing significant tissue destruction.
Types of Lesions
There are several clinical variants of pyoderma gangrenosum, with the ulcerative form being the most common. The ulcerative variant is characterized by the classic painful ulcer with undermined, violaceous borders. Other variants include the bullous form, which presents with superficial vesicles and bullae; the pustular form, associated with inflammatory bowel disease and featuring multiple small pustules; the vegetative form, exhibiting verrucous and ulcerative lesions; and the peristomal form, occurring in the area surrounding a stoma.
RELATED: Nephrogenic Systemic Fibrosis: Guide to Symptoms and Management
Common Sites of Occurrence
While pyoderma gangrenosum can occur anywhere on the body, it most frequently affects the lower extremities, particularly the pretibial area. Other common sites include the upper extremities, trunk, and peristomal regions. In rare cases, pyoderma gangrenosum may involve extracutaneous sites such as the eyes, lungs, and spleen.
Symptoms and Pain Management
Pain is a hallmark feature of pyoderma gangrenosum and can be severe, often described as stabbing or burning in quality. The pain may be disproportionate to the size of the ulcer and can significantly impact a patient’s quality of life. Adequate pain management is crucial in the treatment of pyoderma gangrenosum. Other associated symptoms may include fever, malaise, myalgia, and arthralgia.
The diagnosis of pyoderma gangrenosum is primarily based on clinical features and exclusion of other causes of cutaneous ulceration. Histopathological findings are nonspecific but can help rule out other conditions. It is essential to investigate for associated systemic diseases, as pyoderma gangrenosum is often linked to underlying conditions such as inflammatory bowel disease, arthritis, and hematological disorders.
Diagnostic Challenges and Criteria
Pyoderma gangrenosum is often a diagnosis of exclusion, as there are no definitive diagnostic tests or pathognomonic features. The clinical presentation can mimic other conditions such as infections, vasculitis, and malignancies, leading to misdiagnosis and delayed treatment. A thorough evaluation is necessary to rule out these alternative diagnoses.
Maverakis Criteria
In 2018, Maverakis et al. proposed diagnostic criteria for pyoderma gangrenosum based on a Delphi consensus of international experts. The criteria consist of one major criterion, which is a biopsy of the ulcer edge demonstrating a neutrophilic infiltrate, and eight minor criteria. The minor criteria include the exclusion of infection, pathergy, history of inflammatory bowel disease or inflammatory arthritis, history of a papule, pustule, or vesicle that rapidly ulcerates, peripheral erythema, undermining border, and tenderness at the ulceration site, multiple ulcerations with at least one on the anterior lower leg, cribriform or “wrinkled paper” scars at healed ulcer sites, and decreased ulcer size within one month of initiating immunosuppressive medications. The presence of four or more minor criteria, in addition to the major criterion, yields a sensitivity of 86% and a specificity of 90% for the diagnosis of pyoderma gangrenosum.
RELATED: Managing Nasal Vestibulitis: Key Symptoms and Treatment Plans
Ruling Out Other Conditions
Before a diagnosis of pyoderma gangrenosum can be made, it is crucial to exclude other potential causes of cutaneous ulceration. This process involves a comprehensive evaluation, including a detailed medical history, physical examination, wound cultures, and skin biopsies. Infections, such as bacterial, fungal, and mycobacterial infections, should be ruled out through appropriate cultures and stains. Vasculitis and malignancies, particularly cutaneous T-cell lymphoma, can present with ulcerations similar to pyoderma gangrenosum and should be considered in the differential diagnosis. Histopathological examination of skin biopsies can help to distinguish between these conditions.
Importance of Early Diagnosis
Prompt and accurate diagnosis of pyoderma gangrenosum is essential for optimal patient outcomes. Misdiagnosis can lead to inappropriate treatments, such as surgical debridement or antibiotics, which may exacerbate the condition due to pathergy. Delayed diagnosis and treatment can result in the rapid progression of ulcers, causing significant pain, disfigurement, and a decreased quality of life for patients. Early recognition of pyoderma gangrenosum allows for the timely initiation of appropriate immunosuppressive therapies, which can halt the progression of the disease and promote healing of the ulcers. Therefore, it is crucial for clinicians to maintain a high index of suspicion for pyoderma gangrenosum in patients presenting with rapidly progressing, painful ulcers, particularly in the setting of underlying systemic diseases such as inflammatory bowel disease or rheumatologic conditions.
Comprehensive Treatment Approaches
The mainstay of treatment for pyoderma gangrenosum is immunosuppressive therapy, although there are no definitive guidelines established. Corticosteroids remain the first-line systemic treatment for most patients with PG. Oral prednisone at a dosage of 0.5-1 mg/kg/day can induce a clinical response in up to half of the cases. Once healing is achieved, the corticosteroid dose can be tapered, usually within 6 months. However, it is recommended that systemic corticosteroids be combined with other immunosuppressants or immunomodulatory agents, the most common being cyclosporine.
Corticosteroids and Immunosuppressants
The choice between prednisolone and cyclosporine depends on patients’ comorbidities. Pre-existing conditions favoring prednisolone over cyclosporine include renal insufficiency, malignancy, and hypertension, whereas patients with obesity, diabetes, osteoporosis, peptic ulcer disease, or a history of mental illness may benefit from using cyclosporine rather than prednisolone. Mycophenolate mofetil has also demonstrated efficacy and safety in treating PG, even in severe, tendon-exposing, refractory cases. It can be used as an adjunct to corticosteroids or as a steroid-sparing agent.
Biologic Agents
In recent years, biologic agents have expanded the treatment options for PG, with tumor necrosis factor-alpha (TNF-α) inhibitors being the best supported in the literature. Infliximab and adalimumab have shown higher response rates compared to other TNF-α inhibitors. These biologics can be particularly beneficial in patients with underlying inflammatory comorbidities such as inflammatory bowel disease. Emerging evidence also supports the use of other biologic agents targeting interleukin (IL)-12, IL-23, IL-1, and IL-6.
Surgical Interventions and Considerations
Surgical interventions such as split-thickness skin grafting (STSG) and negative pressure wound therapy (NPWT) have been controversial in the management of PG due to the risk of pathergy. However, recent advances confirm that a surgical approach with STSG secured by NPWT is a safe and valuable treatment option if performed under adequate immunosuppression. NPWT alone, without skin grafting, may halt the inflammatory process but does not significantly accelerate healing time. The best surgical approach appears to be STSG fixed with NPWT, as this leads to higher skin graft take.
It is crucial to note that PG has a chronic nature, and recurrence may occur after tapering immunosuppression or trauma. Therefore, sustained immunosuppressive treatment is suggested. A multidisciplinary approach involving wound care specialists, dermatologists, and surgeons is essential for optimal patient outcomes in the management of pyoderma gangrenosum.
Living with Pyoderma Gangrenosum
Living with pyoderma gangrenosum can be challenging, as the condition has a significant impact on a patient’s quality of life. The chronic, painful ulcers and the unpredictable course of the disease often lead to physical limitations, emotional distress, and social isolation.
Coping Strategies
Developing effective coping strategies is crucial for individuals with pyoderma gangrenosum. Patients should work closely with their healthcare team to manage pain, which is a major factor affecting daily activities and sleep. Relaxation techniques, such as deep breathing exercises or meditation, may help alleviate stress and promote a sense of well-being. Engaging in gentle physical activities, as tolerated, can improve mood and overall health.
RELATED: Mitral Valve Prolapse: From Symptoms to Treatment Options
Preventing Complications
Preventing complications is a key aspect of living with pyoderma gangrenosum. Patients should follow their treatment plan diligently and attend regular follow-up appointments to monitor their condition. Proper wound care is essential to reduce the risk of infection and promote healing. This may involve using non-adherent dressings, cleansing the wound regularly, and protecting the affected area from further trauma. Patients should also be vigilant for signs of infection, such as increased pain, redness, swelling, or discharge, and report these to their healthcare provider promptly.
Support and Resources
Seeking support is vital for individuals living with pyoderma gangrenosum. Patients may benefit from joining a support group, either in-person or online, to connect with others who have similar experiences. Sharing their journey and learning from others can provide a sense of community and reduce feelings of isolation. Additionally, patients should be encouraged to reach out to mental health professionals if they experience persistent feelings of depression, anxiety, or difficulty coping with their condition. Family and friends can also play a crucial role in providing emotional support and practical assistance with daily tasks.
Conclusion
Pyoderma gangrenosum is a rare and challenging skin condition that can have a significant impact on a person’s quality of life. This painful, ulcerative disorder often starts as small pustules or nodules that rapidly progress to deep, destructive lesions. Despite its name, pyoderma gangrenosum is neither infectious nor gangrenous, making its diagnosis and treatment complex for healthcare professionals.
Understanding pyoderma gangrenosum is crucial for both patients and medical practitioners. This article aims to shed light on the key aspects of this condition, including its clinical presentation, diagnostic challenges, and comprehensive treatment approaches. It will also explore the day-to-day realities of living with pyoderma gangrenosum, providing valuable insights for those affected by this often misunderstood skin disorder.