Sarcoma, a rare and complex group of cancers, affects thousands of people worldwide each year. This type of cancer develops in the body’s connective tissues, including bones, muscles, tendons, and fat. Despite its rarity, sarcoma has a significant impact on those diagnosed, making early detection and proper treatment crucial for improving outcomes and quality of life.
Understanding sarcoma is essential for patients, caregivers, and healthcare professionals alike. This article aims to provide a comprehensive overview of sarcoma, covering its basic characteristics, warning signs, diagnostic processes, and treatment strategies. By exploring these aspects, readers will gain valuable insights to recognize symptoms early and navigate the available treatment options more effectively.
Sarcoma Basics



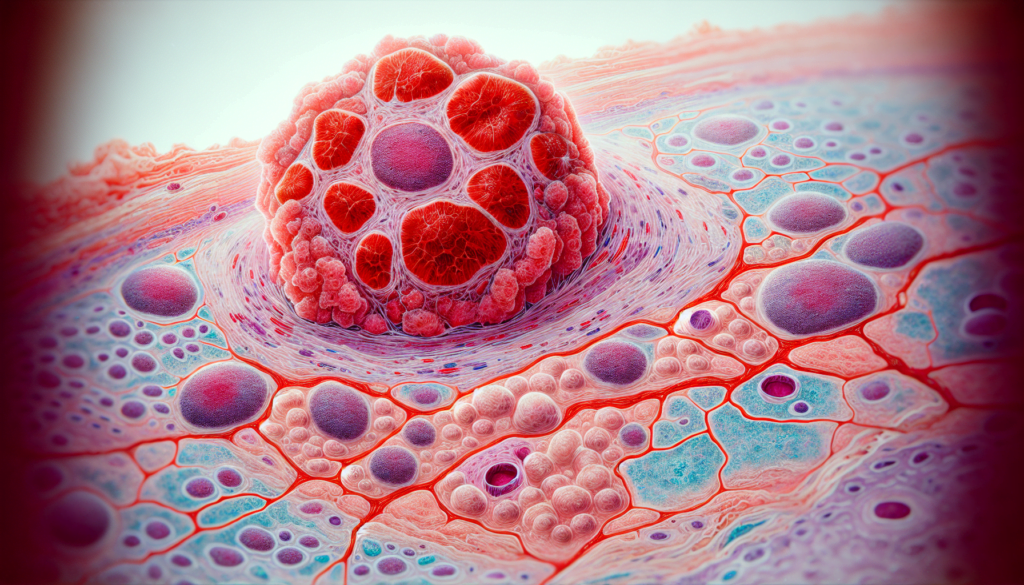
Sarcoma is a rare and complex type of cancer that develops in the body’s connective tissues, such as bones, muscles, tendons, and fat. It affects thousands of people worldwide each year, with around 3,300 people diagnosed with soft tissue sarcoma in the UK in 2010. Despite its rarity, sarcoma has a significant impact on those diagnosed, making early detection and proper treatment crucial for improving outcomes and quality of life.
There are two main types of sarcoma: soft tissue sarcoma and bone sarcoma. Soft tissue sarcoma is the most common, developing in the soft tissues of the body, usually the muscles or blood vessels. Bone sarcoma, on the other hand, forms in the bone and is less common.
Within these two main types, there are more than 70 different subtypes of sarcoma, classified based on where in the soft tissue or bone the cancer originated. Some of the most common subtypes include:
- Angiosarcoma (vascular sarcoma)
- Chondrosarcoma
- Clear cell sarcoma
- Dermatofibrosarcoma protuberans (DFSP)
- Epithelioid sarcoma
- Ewing’s sarcoma
- Fibrosarcoma (fibroblastic sarcoma)
- Gastrointestinal stromal tumors (GIST)
- Kaposi sarcoma
- Leiomyosarcoma
- Liposarcoma
- Osteosarcoma
- Pleomorphic sarcoma
- Rhabdomyosarcoma
- Spindle cell sarcoma
- Synovial sarcoma
RELATED: Vasculitis Explained: Key Symptoms and Treatment Options
The risk of developing sarcoma depends on various factors, including age, genetics, lifestyle, and environmental factors. While the exact causes of most soft tissue sarcomas are unknown, certain factors may increase the risk, such as:
- Age (40% of soft tissue sarcomas are diagnosed in people aged 65 or older)
- Previous radiotherapy treatment
- Exposure to certain chemicals (e.g., radioiodines, polychlorophenols)
- Family history of rare genetic conditions (e.g., neurofibromatosis, Li Fraumeni syndrome, retinoblastoma)
- Infections and lowered immunity (e.g., Human Herpes Virus 8, Epstein Barr virus)
- Chronic lymphedema following breast removal or in the leg
It is important to note that having any of these risk factors does not necessarily mean that an individual will develop sarcoma. However, understanding these factors can help raise awareness and promote early detection and intervention.
Recognizing Warning Signs
Recognizing the early warning signs of sarcoma is crucial for prompt diagnosis and treatment. Sarcoma symptoms can vary depending on the location and size of the tumor, but there are some common signs to watch out for.
One of the first symptoms of sarcoma is often a painless lump or swelling in the soft tissue or bone. This lump may grow over time and can be felt under the skin. In some cases, the lump may cause pain if it presses on nerves or muscles.
Other symptoms of sarcoma may include:
- Pain in the affected area, especially if it worsens over time
- Swelling or stiffness in a joint
- Difficulty walking or reduced range of motion
- Unexplained fatigue, reduced appetite, or unintended weight loss
- Abdominal pain, constipation, or bloody stools (for sarcomas in the abdomen)
RELATED: Toxoplasmosis: Effective Treatment Methods and Prevention Tips
Soft tissue sarcomas and bone sarcomas can present with different signs and symptoms. Soft tissue sarcomas are typically painless when they first develop, and patients may only experience symptoms once the tumor has grown large enough to affect nearby structures. Bone sarcomas, on the other hand, often cause pain as an early symptom.
Early detection of sarcoma is vital for improving outcomes and quality of life. The NHS recommends assessment of any lump that is larger than 5cm, deep, rapidly growing, painful, or recurrent. If you notice any persistent or worsening symptoms, it is essential to consult a healthcare professional promptly for further evaluation, which may include physical examination, imaging tests, and biopsy.
By being aware of the warning signs and seeking early medical attention, patients can increase their chances of successful treatment and recovery from sarcoma.
Diagnostic Journey
The diagnostic journey for sarcoma involves a series of steps to accurately identify the presence and type of sarcoma. The process begins with an initial consultation with a healthcare professional, followed by imaging tests and a biopsy for a definitive diagnosis.
During the initial consultation, the doctor will review the patient’s medical history and conduct a physical examination. They will assess any lumps or swellings, checking their size, shape, and texture. The doctor may also evaluate the patient’s range of motion and check for any signs of weakness or abnormalities in the lungs or abdomen.
Imaging tests play a crucial role in diagnosing sarcoma. MRI scans are commonly used to examine lumps in the arms or legs, providing detailed images of the tumor’s size, location, and surrounding tissues. CT scans are often used to assess lumps in the abdomen, retroperitoneum, and chest, as well as to check for metastasis. Ultrasound may be used to determine if a lump is a solid tumor or a fluid-filled cyst, while X-rays can help examine lumps and bone lesions.
RELATED: Everything You Should Know About Tourette Syndrome
If imaging tests suggest the presence of a sarcoma, a biopsy is performed to confirm the diagnosis and determine the specific type of sarcoma. Core needle biopsy and surgical biopsy are common techniques used to obtain tissue samples. The samples are then analyzed by a pathologist, who examines them under a microscope and conducts additional tests to identify the sarcoma type and grade.
The diagnostic process for sarcoma can be complex and time-consuming, often requiring the expertise of specialists at a large cancer center. It is essential for patients to work closely with their healthcare team throughout the diagnostic journey to ensure accurate results and appropriate treatment planning.
Comprehensive Treatment Strategies
Sarcoma treatment involves a multidisciplinary approach, with specialists from various fields collaborating to provide optimal care. The treatment plan depends on factors such as the sarcoma type, stage, location, and the patient’s overall health.
Surgery is the primary treatment for most sarcomas, aiming to remove the tumor with clear margins. Limb-sparing surgery is preferred whenever possible, but amputation may be necessary in some cases. Radiation therapy can be used before or after surgery to shrink the tumor or reduce the risk of recurrence. It may also be the main treatment for inoperable tumors.
Chemotherapy is often used for high-grade sarcomas to reduce the risk of metastasis. The most common regimens include doxorubicin, and combination therapies. Targeted therapies for gastrointestinal stromal tumors (GIST), have improved outcomes for specific sarcoma subtypes.
Treatment strategies vary by stage:
- Stage I: Surgery alone may be sufficient for low-grade, localized tumors.
- Stage II-III: A combination of surgery, radiation, and/or chemotherapy is typically used for high-grade or larger tumors.
- Stage IV: Treatment focuses on controlling symptoms and extending survival, using a combination of surgery, radiation, chemotherapy, and targeted therapies.
Emerging therapies, such as immunotherapy and precision medicine, are showing promise in sarcoma treatment. Immune checkpoint inhibitors, have demonstrated efficacy in some sarcoma subtypes. Targeted therapies based on the tumor’s molecular profile are also being developed, offering hope for personalized treatment approaches.
Ongoing clinical trials are crucial for improving sarcoma outcomes, and patients should be encouraged to participate whenever possible. A multidisciplinary team, including orthopedic oncologists, surgical oncologists, medical oncologists, radiation oncologists, pathologists, and radiologists, is essential for providing comprehensive, coordinated care throughout the treatment journey.
Conclusion
Sarcoma, a rare and complex cancer affecting connective tissues, has a significant impact on those diagnosed. Early detection and proper treatment are key to improving outcomes and quality of life for patients. Understanding the warning signs, diagnostic process, and available treatments empowers individuals to take action and seek medical attention promptly. This knowledge can make a real difference in managing this challenging disease.
The fight against sarcoma continues to evolve, with ongoing research and clinical trials paving the way for new therapies and personalized treatment approaches. Multidisciplinary care teams play a crucial role in providing comprehensive support throughout the patient’s journey. By raising awareness and promoting education about sarcoma, we can help to ensure earlier diagnoses and better outcomes for those affected by this rare but impactful cancer.