Scoliosis, a condition characterized by an abnormal curvature of the spine, affects millions of people worldwide. This spinal deformity can cause pain, limit mobility, and even impact breathing in severe cases. Understanding scoliosis is crucial for early detection and effective management, as it can develop at any age but often begins during childhood or adolescence.
This article aims to provide a comprehensive look at scoliosis, covering its various types and symptoms. It will explore the causes and risk factors associated with this condition, shedding light on both genetic and environmental influences. Additionally, the piece will delve into the diagnosis and assessment methods used by healthcare professionals to identify and evaluate scoliosis. By examining these aspects, readers will gain valuable insights into this complex spinal disorder and its impact on those affected.
Understanding Scoliosis: Types and Symptoms



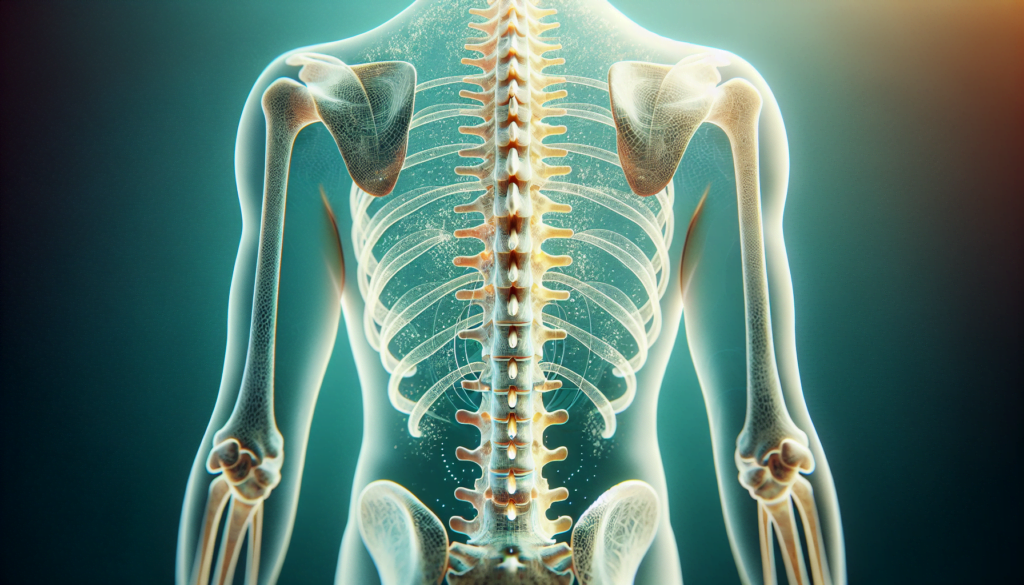
Scoliosis is an abnormal sideways curvature of the spine that can occur in various patterns and degrees of severity. While scoliosis is often first diagnosed in children, it can affect individuals of any age. The condition is characterized by a C- or S-shaped curve in the spine, which may also involve a rotation of the vertebrae.
Definition of Scoliosis
Scoliosis is determined when the curvature of the spine measures 10 degrees or greater on an X-ray. The curvature can occur on the right or left side of the spine, or on both sides in different sections, and may affect both the thoracic (mid) and lumbar (lower) regions of the spine.
Types of Scoliosis
There are several types of scoliosis, each with its own characteristics and causes:
- Idiopathic Scoliosis: The most common type, accounting for about 80% of cases. The cause is unknown, but it is believed to have a genetic component. Idiopathic scoliosis is further categorized by age of onset:
- Infantile Idiopathic Scoliosis (age 0-3)
- Juvenile Idiopathic Scoliosis (age 4-10)
- Adolescent Idiopathic Scoliosis (age 11-18)
- Adult Idiopathic Scoliosis (age 18+)
- Congenital Scoliosis: A rare form that develops due to vertebral malformations during fetal development. It may be detected at birth or later in childhood.
- Neuromuscular Scoliosis: Occurs in individuals with underlying neuromuscular conditions such as cerebral palsy, muscular dystrophy, or spina bifida. Weak or imbalanced muscles lead to the development of spinal curvature.
- Degenerative Scoliosis: Develops later in life as a result of wear and tear on the spine, often associated with conditions like arthritis or osteoporosis.
RELATED: Understanding Aphallia: Causes, Symptoms, and Treatments
Common Symptoms and Signs
Most cases of scoliosis are mild and do not cause noticeable symptoms. However, some common signs and symptoms may include:
- Uneven shoulders, waist, or hips
- One shoulder blade appearing more prominent than the other
- Ribs protruding more on one side when bending forward
- Visible curve in the spine
- Leaning to one side
- Back pain (in severe cases)
- Difficulty breathing (in severe cases)
It is important to note that the presence of one or more of these signs does not necessarily indicate scoliosis. A proper diagnosis by a healthcare professional is required to confirm the condition and determine its severity. Early detection and intervention are crucial for the successful management of scoliosis and the prevention of potential complications.
Causes and Risk Factors of Scoliosis
Scoliosis has an influence on the spine, causing it to curve sideways into a “C” or “S” shape. The causes and risk factors vary depending on the type of scoliosis. Let’s explore the different types and their associated causes.
Idiopathic Scoliosis
Idiopathic scoliosis is the most common type, accounting for about 80% of cases. The cause is unknown, but it is believed to have a genetic component. Idiopathic scoliosis is further categorized by age of onset:
- Infantile Idiopathic Scoliosis (age 0-3)
- Juvenile Idiopathic Scoliosis (age 4-10)
- Adolescent Idiopathic Scoliosis (age 11-18)
- Adult Idiopathic Scoliosis (age 18+)
Congenital Scoliosis
Congenital scoliosis is a rare form that develops due to vertebral malformations during fetal development. It may be detected at birth or later in childhood. Congenital scoliosis occurs early in pregnancy, when one or more of the vertebrae in the spine don’t form completely. This can cause a sharp angle — called a hemivertebrae — to develop in the spine.
RELATED: Understanding Aquaphobia: Causes, Symptoms, and Treatment Options
Neuromuscular Scoliosis
Neuromuscular scoliosis occurs in individuals with underlying neuromuscular conditions such as cerebral palsy, muscular dystrophy, or spina bifida. Weak or imbalanced muscles lead to the development of spinal curvature. Neuromuscular scoliosis is caused by poor muscle control, weakness or paralysis, and neurological problems associated with the underlying conditions.
Genetic Factors
While the exact cause of idiopathic scoliosis is unknown, research indicates that it runs in families and has a genetic link. Having a parent or sibling with scoliosis increases a person’s chances of having scoliosis too. Twin studies have consistently shown higher concordance in monozygotic compared to dizygotic twins, indicating a genetic influence.
In summary, scoliosis can be caused by a variety of factors, including congenital malformations, neuromuscular disorders, and genetic predisposition. Understanding the underlying causes and risk factors is crucial for early detection, effective management, and prevention of potential complications associated with scoliosis.
Diagnosis and Assessment of Scoliosis
Diagnosing scoliosis involves a combination of physical examination and imaging tests to assess the severity and type of spinal curvature. Healthcare professionals use these methods to determine the best course of treatment for each individual patient.
Physical Examination
The first step in diagnosing scoliosis is a physical examination. During this examination, the healthcare provider will assess the patient’s posture, shoulders, hips, and waistline for any visible asymmetry. They may also perform the Adam’s forward bend test, which involves the patient bending forward at the waist with their arms hanging loosely. This test allows the examiner to observe any unevenness in the rib cage or the presence of a rib hump, which can indicate scoliosis.
In addition to the visual assessment, the healthcare provider may use a scoliometer, a specialized tool that measures the angle of trunk rotation (ATR). An ATR of 5 degrees or more may warrant further investigation through imaging tests.
Imaging Tests
Imaging tests play a crucial role in confirming the diagnosis of scoliosis and determining the severity of the spinal curvature. The most common imaging test used is a standing posteroanterior (PA) radiograph of the spine. This X-ray provides a clear view of the spine and allows for the measurement of the Cobb angle, which quantifies the degree of curvature.
In some cases, additional imaging tests may be necessary, such as:
- Lateral radiographs: These X-rays provide a side view of the spine and can help assess the sagittal alignment and any associated kyphosis or lordosis.
- Magnetic Resonance Imaging (MRI): An MRI may be ordered if there are concerns about spinal cord abnormalities or underlying neurological conditions that could be causing the scoliosis.
- Computed Tomography (CT) scans: CT scans can provide detailed images of the vertebrae and may be used in cases of congenital scoliosis or to assess the bony anatomy prior to surgical intervention.
RELATED: Aquagenic Pruritus: Causes, Symptoms, and Relief Strategies
Measuring Curve Severity
The severity of scoliosis is primarily determined by measuring the Cobb angle on the PA radiograph. The Cobb angle is formed by drawing lines parallel to the upper and lower endplates of the most tilted vertebrae at the top and bottom of the curve. The angle between these lines is the Cobb angle.
The severity of scoliosis is classified based on the Cobb angle:
| Cobb Angle | Severity Classification |
|---|---|
| 10-20° | Mild |
| 20-40° | Moderate |
| >40° | Severe |
In addition to the Cobb angle, healthcare providers also consider factors such as skeletal maturity, curve location, and curve pattern when assessing the severity and prognosis of scoliosis. The Risser sign, which indicates the degree of iliac crest ossification, is often used to determine skeletal maturity and the likelihood of curve progression.
Accurate diagnosis and assessment of scoliosis are essential for developing an appropriate treatment plan. By combining physical examination findings with imaging tests and measurements of curve severity, healthcare professionals can provide personalized care to patients with scoliosis, aiming to prevent progression, alleviate symptoms, and improve overall quality of life.
Conclusion
Scoliosis has a significant impact on the lives of millions worldwide, affecting people of all ages. This complex spinal disorder presents various challenges, from mild cases that require monitoring to severe instances needing surgical intervention. Understanding the different types, causes, and diagnostic methods is crucial to manage this condition effectively. Early detection and proper assessment play a key role in developing tailored treatment plans, aiming to improve patients’ quality of life.
As research in this field continues, new insights into the genetic factors and potential treatments are emerging. These advancements offer hope for better management strategies and possibly even preventive measures in the future. For those affected by scoliosis, staying informed about the latest developments and working closely with healthcare professionals can make a real difference in their journey to cope with and overcome the challenges posed by this condition.