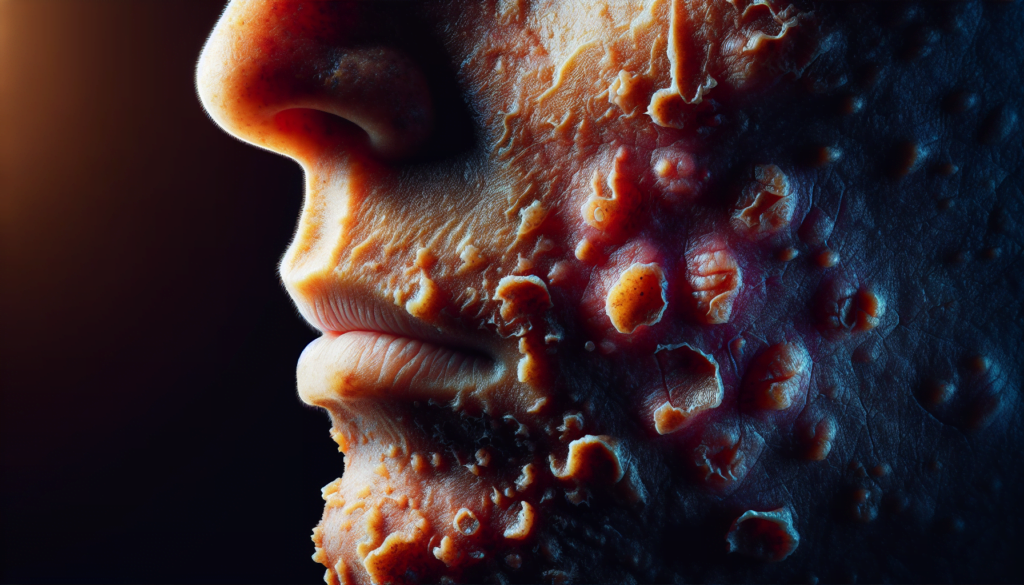
Stevens-Johnson Syndrome is a rare but severe skin reaction that can be life-threatening. This condition affects the skin and mucous membranes, causing a painful rash, blisters, and shedding of the skin. It often starts with flu-like symptoms before progressing to more serious manifestations. Stevens-Johnson Syndrome is typically triggered by certain medications or infections, making it crucial to recognize early warning signs and seek immediate medical attention.
Understanding Stevens-Johnson Syndrome is essential for both healthcare professionals and the general public. This article aims to provide a comprehensive overview of the condition, covering its diagnosis, treatment approaches, and potential long-term effects. By exploring the causes, symptoms, and management strategies, readers will gain valuable insights into this serious medical condition. The information presented will help to raise awareness and promote early intervention, which can significantly improve outcomes for those affected by Stevens-Johnson Syndrome.
Diagnosis of Stevens-Johnson Syndrome



The diagnosis of Stevens-Johnson syndrome (SJS) involves a combination of a thorough medical history, physical examination, and diagnostic tests. Healthcare providers can often identify SJS based on the patient’s medical history, including a review of current and recently stopped medications, and a physical exam.
Medical History and Physical Examination
A comprehensive medical history is crucial in diagnosing SJS. The healthcare provider will inquire about the onset and progression of symptoms, recent illnesses, and any medications the patient has been taking. They will also perform a physical examination, focusing on the skin, mucous membranes, and other affected areas.
Skin Biopsy
To confirm the diagnosis and rule out other possible causes, a skin biopsy may be performed. The healthcare provider will remove a small sample of affected skin for laboratory testing. The biopsy can help differentiate SJS from other conditions with similar presentations.
RELATED: Living with Amyotrophic Lateral Sclerosis (ALS): What You Need to Know
Laboratory Tests
Various laboratory tests may be conducted to aid in the diagnosis of SJS and to assess the patient’s overall health:
- Culture: To rule out an infection, a sample of skin, tissue, or fluid may be taken for laboratory testing (culture).
- Imaging: Depending on the patient’s symptoms, imaging tests such as a chest X-ray may be performed to check for complications like pneumonia.
- Blood tests: These tests can help confirm the presence of an infection or other possible causes. They may include a complete blood count (CBC), liver function tests (LFTs), and electrolyte levels.
The diagnosis of SJS requires a high index of suspicion and a thorough evaluation of the patient’s medical history, physical findings, and diagnostic test results. Early recognition and prompt treatment are essential to minimize complications and improve patient outcomes.
Treatment Approaches
Treatment of Stevens-Johnson syndrome (SJS) requires hospitalization, often in an intensive care unit or burn unit. The primary goals are to identify and discontinue the offending medication, provide supportive care, and prevent complications.
Supportive Care
Supportive care is the cornerstone of SJS treatment. This includes:
- Fluid replacement and nutrition: Patients with SJS experience significant fluid loss through the skin and may require intravenous fluids and electrolyte replacement. Nutritional support through a nasogastric tube may be necessary.
- Wound care: Gentle removal of necrotic skin and mucosal tissue, along with the application of non-adherent dressings and topical antiseptics, helps prevent infection and promote healing.
- Temperature control: Maintaining a warm environment and using heat shields or infrared lamps can help reduce heat loss through the affected skin.
- Pain management: Adequate pain relief is essential, as SJS can be extremely painful.
Medication Management
While the offending medication must be discontinued immediately, additional medications may be necessary to manage symptoms and prevent complications:
- Antibiotics: Although prophylactic systemic antibiotics are not recommended, they may be necessary if secondary infections develop.
- Corticosteroids: The use of systemic corticosteroids remains controversial. Some studies suggest that short-term, high-dose intravenous corticosteroids may be beneficial when administered early in the course of the disease.
- Immunomodulatory agents: Intravenous immunoglobulin (IVIG) has shown promise in blocking the Fas-Fas ligand mediated apoptosis in keratinocytes when administered at high doses early in the course of SJS.
RELATED: Understanding Trypophobia: Causes, Symptoms, and Treatments
Specialized Care for Affected Areas
Specific management strategies are required for the various areas affected by SJS:
- Ocular care: Aggressive lubrication of the ocular surface, topical steroids, and antibiotics are used to manage acute ocular manifestations. Amniotic membrane grafting may be necessary to maintain ocular integrity.
- Oral care: Mouthwashes and topical anesthetics can help manage oral lesions and reduce pain, allowing for better fluid intake.
- Respiratory care: In severe cases, mechanical ventilation may be necessary due to respiratory tract involvement.
Long-term follow-up and management are essential, as SJS can result in significant sequelae, particularly in the eyes. Patients should be advised to avoid the causative medication and structurally related drugs to prevent recurrence.
Complications and Long-Term Effects
Stevens-johnson syndrome (SJS) can lead to severe complications and long-term effects that significantly impact the quality of life of affected individuals. The most common complications involve the eyes, respiratory system, and psychological well-being.
Ocular complications are among the most devastating consequences of SJS. In the acute phase, patients may experience conjunctivitis, corneal ulceration, and even corneal perforation. Long-term ocular sequelae include:
- Symblepharon formation
- Corneal scarring and neovascularization
- Limbal stem cell deficiency
- Chronic dry eye syndrome
These complications can result in severe visual impairment and, in some cases, complete loss of vision.
Respiratory issues are another significant concern in SJS patients. During the acute phase, mucosal sloughing can occur in the respiratory tract, leading to airway obstruction and respiratory failure. Long-term respiratory complications may include:
- Bronchiolitis obliterans
- Interstitial lung disease
- Chronic cough and dyspnea
These respiratory sequelae can have a profound impact on the patient’s quality of life and may require ongoing medical management.
The psychological impact of SJS cannot be overstated. Patients often experience significant emotional distress due to the acute illness, prolonged hospitalization, and long-term complications. Common psychological issues include:
- Depression
- Anxiety
- Post-traumatic stress disorder (PTSD)
Patients may struggle with changes in their appearance, loss of independence, and the need for ongoing medical care. Psychological support and counseling are essential components of the long-term management of SJS patients.
RELATED: Tonsillitis Explained: From Symptoms to Effective Remedies
| Complication | Acute Phase | Long-Term Effects |
|---|---|---|
| Ocular | Conjunctivitis, corneal ulceration, perforation | Symblepharon, corneal scarring, limbal stem cell deficiency, dry eye |
| Respiratory | Mucosal sloughing, airway obstruction, respiratory failure | Bronchiolitis obliterans, interstitial lung disease, chronic cough and dyspnea |
| Psychological | Emotional distress, prolonged hospitalization | Depression, anxiety, PTSD |
In conclusion, the complications and long-term effects of Stevens-johnson syndrome can have a profound impact on the lives of affected individuals. Close monitoring, ongoing medical management, and psychological support are essential to minimize the burden of these sequelae and improve the overall quality of life for SJS survivors.
Conclusion
Stevens-Johnson Syndrome is a serious medical condition that has a significant impact on patients’ lives. This comprehensive overview has shed light on its diagnosis, treatment approaches, and potential long-term effects. By understanding the causes and symptoms, healthcare providers and the public can work together to spot early warning signs and take quick action, which is crucial to improve outcomes for those affected.
To wrap up, raising awareness about Stevens-Johnson Syndrome is key to promote early intervention and better management of this rare but severe skin reaction. The information presented in this article aims to equip readers with valuable insights to understand and navigate this challenging condition. Remember, while Stevens-Johnson Syndrome can be life-threatening, proper care and ongoing support can help patients manage its effects and maintain a good quality of life.