Toothache can be an excruciating experience, often disrupting daily life and causing significant discomfort. This common dental issue affects millions of people worldwide, ranging from mild sensitivity to severe, throbbing pain. Understanding the causes and available treatments for toothaches is crucial for maintaining oral health and preventing further complications.
This article delves into the various aspects of toothaches, providing expert advice on identifying symptoms and exploring effective treatment options. Readers will gain insights into the common causes of dental pain, learn about professional interventions, and discover preventive measures to reduce the risk of future toothaches. By the end, they’ll be equipped with valuable knowledge to address and manage this prevalent dental concern.
Common Causes of Toothaches


Toothaches can have various underlying causes, ranging from minor issues to serious dental problems. Understanding these common causes can help individuals identify the source of their discomfort and seek appropriate treatment.
Tooth Decay
Tooth decay, also known as cavities, is one of the most prevalent causes of toothaches. When bacteria in the mouth feed on sugars and starches, they produce acid that erodes tooth enamel. Over time, this erosion can create small openings or holes in the teeth, exposing the sensitive inner layers and leading to pain. Regular dental check-ups and good oral hygiene practices, such as brushing with fluoride toothpaste and flossing, can help prevent and detect tooth decay early on.
Dental Abscess
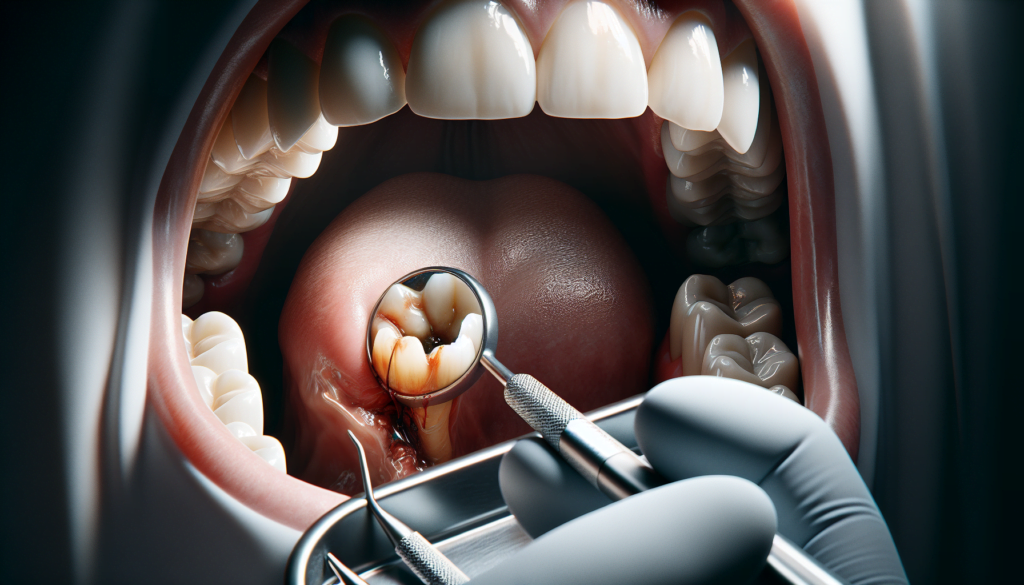
A dental abscess is a pocket of pus that forms at the root of a tooth or in the gums. It occurs when bacteria invade the pulp, the innermost part of the tooth containing nerves and blood vessels. Abscesses can cause severe, throbbing pain, swelling, and sensitivity to temperature. They require prompt treatment from a dentist, who may perform a root canal or extract the affected tooth to prevent the infection from spreading.
Cracked or Chipped Tooth
Trauma to a tooth, such as from biting on hard objects or experiencing a blow to the face, can result in cracks or chips. These injuries can expose the tooth’s sensitive inner layers, leading to pain and discomfort. Depending on the extent of the damage, treatment options may include dental bonding, crowns, or root canal therapy. Wearing a mouthguard during sports activities and avoiding habits like chewing on ice can help prevent tooth injuries.
RELATED: Neutropenia: How to Recognize and Manage Low Neutrophil Counts
Gum Disease
Gum disease, or periodontal disease, is an infection of the tissues surrounding the teeth. In its early stages, known as gingivitis, it can cause red, swollen, and bleeding gums. If left untreated, it can progress to periodontitis, a more severe form that can lead to receding gums, bone loss, and toothaches. Regular dental cleanings, proper brushing and flossing techniques, and managing risk factors like smoking and diabetes can help prevent and manage gum disease.
Identifying Toothache Symptoms
Types of Pain
Toothaches can manifest in various ways, each indicating a different underlying issue. A dull, lingering ache is the most common type of toothache, often caused by food stuck between teeth, an abscessed tooth, or bruxism. Sensitivity to hot or cold temperatures may signify worn enamel, tooth decay, cracks, exposed roots, or gum disease. Sharp or jabbing pain usually requires a dentist’s attention, as it can be due to a loose filling, a fallen crown, a fracture, or a cavity. Severe, throbbing pain that becomes distracting or intolerable warrants an emergency dental visit, especially if accompanied by discolored gums, bleeding gums, or a strange taste in the mouth.
Associated Symptoms
In addition to pain, toothaches may present with other symptoms that can help pinpoint the cause. Swelling in the face, cheek, or neck can indicate an infection and may lead to difficulty breathing or swallowing. Tender, swollen lymph nodes under the jaw or in the neck are another sign of infection. A foul odor or taste in the mouth may suggest an abscessed tooth or advanced decay. If the abscess ruptures, a sudden rush of foul-smelling and foul-tasting fluid may fill the mouth, providing temporary pain relief.
When to Seek Professional Help
While some toothaches may be managed temporarily with home remedies, it’s crucial to seek professional dental care to address the underlying issue. If a toothache lasts longer than two days, is accompanied by swelling in the face or jaw, or causes pain when opening the mouth wide, it’s time to see a dentist. Severe pain that doesn’t improve with over-the-counter medications, bleeding that won’t stop with applied pressure, or a fever over 101 degrees Fahrenheit (38.33 degrees Celsius) warrant an emergency dental visit or a trip to the emergency room if outside of dental office hours. Prompt treatment can prevent the spread of infection and further complications.
Professional Treatments for Toothaches
Dental Fillings
When tooth decay has progressed to the point of forming a cavity, dental fillings become necessary. The dentist removes the decayed portion of the tooth using a high-speed drill and fills the resulting hole with a filling material. Common filling materials include amalgam, composite resin, and glass ionomer. The choice of material depends on factors such as the location and extent of the decay, as well as the patient’s preferences. Once the filling is placed, the dentist shapes it to match the contours of the tooth and ensures a proper bite alignment.
Root Canal Therapy
If a toothache is caused by an infection that has reached the pulp (the innermost part of the tooth containing nerves and blood vessels), root canal therapy may be required. During this procedure, the dentist or endodontist removes the infected pulp, cleans and shapes the root canals, and fills them with a biocompatible material called gutta-percha. The tooth is then sealed and often restored with a crown to protect it from further damage. Root canal therapy is an effective way to save a severely infected tooth that would otherwise require extraction.
RELATED: Exploring Necrotizing Fasciitis: What You Should Know
Tooth Extraction
In some cases, a tooth may be too badly damaged or decayed to be saved, and extraction becomes necessary. The dentist numbs the area around the tooth with local anesthesia and then uses specialized instruments to loosen and remove the tooth from its socket. After the extraction, the dentist provides instructions for care, which may include biting on a gauze pad to control bleeding and avoiding hard or crunchy foods during the healing process. In some cases, the dentist may recommend replacing the extracted tooth with a dental implant, bridge, or denture to restore function and prevent neighboring teeth from shifting.
Antibiotics
When a toothache is accompanied by signs of infection, such as swelling, fever, or severe pain, the dentist may prescribe antibiotics to help control the spread of bacteria. Antibiotics are usually given in combination with other treatments, such as root canal therapy or tooth extraction, to address the underlying cause of the infection. It is important to take antibiotics as directed and to finish the entire course, even if symptoms improve, to prevent the development of antibiotic-resistant bacteria. Patients should also be aware that antibiotics may cause side effects, such as digestive issues or allergic reactions, and should report any concerns to their dentist or healthcare provider.
Preventing Future Toothaches
Good oral hygiene is the key to preventing toothaches. Brushing twice daily with fluoride toothpaste and flossing at least once a day removes plaque and food particles that can lead to tooth decay. Using an antibacterial mouthwash can also help reduce harmful bacteria in the mouth.
Regular dental check-ups are crucial for maintaining oral health. During these visits, dentists can identify and treat potential issues before they develop into painful toothaches. Professional cleanings remove tartar and plaque buildup that brushing and flossing may miss.
RELATED: Necrosis Explained: Causes, Symptoms, and Treatment Options
Diet plays a significant role in tooth health. Limiting sugary and acidic foods and drinks can help prevent tooth decay. Sticky foods like candy and dried fruit can cling to teeth, providing fuel for cavity-causing bacteria. Incorporating crunchy fruits and vegetables into the diet stimulates saliva production, which helps neutralize acids and wash away food particles.
Wearing a mouthguard during sports activities and avoiding habits like chewing on ice or hard objects can prevent tooth injuries that lead to toothaches. For those who grind their teeth at night, a custom-fitted night guard from a dentist can protect teeth from excessive wear and sensitivity.
Conclusion
Toothaches can have a significant impact on daily life, causing discomfort and disrupting regular activities. Understanding the root causes, recognizing symptoms, and knowing when to seek professional help are crucial steps to manage and prevent dental pain. By maintaining good oral hygiene, attending regular check-ups, and being mindful of dietary choices, individuals can take proactive measures to reduce the risk of future toothaches.
While home remedies may provide temporary relief, professional dental care is often necessary to address the underlying issues causing toothaches. Dentists offer a range of treatments, from simple fillings to more complex procedures like root canals or extractions, tailored to each patient’s specific needs. By staying informed and taking action early, people can protect their oral health and enjoy a pain-free smile for years to come.