Arachnoid cysts, benign fluid-filled sacs that can occur within the cranial space and on the arachnoid membrane—one of the three membranes that cover the brain and spinal cord—pose a puzzling medical phenomenon. While they often remain asymptomatic and are discovered incidentally during radiological examinations for unrelated issues, understanding what is an arachnoid cyst, its potential impact on health, and its indication of underlying conditions is of paramount importance. Due to advancements in arachnoid cysts radiology, the detection and diagnosis rates have significantly increased, bringing attention to their management and the need for research on arachnoid cyst causes and arachnoid cysts treatment options.
This article delves into the intricate world of arachnoid cysts, exploring their causes and risk factors, identifying the various arachnoid cyst symptoms in adults and children, and discussing the innovative diagnostic methods available. Treatment options for arachnoid cysts range from watchful waiting in asymptomatic cases to surgical interventions for those presenting significant symptoms or complications. By unpacking the complexities surrounding arachnoid cyst brain conditions, including potential complications and the prognosis after treatment, readers will gain a comprehensive understanding of these cysts, aiding in the destigmatization of the condition and promoting informed discussions on management strategies.
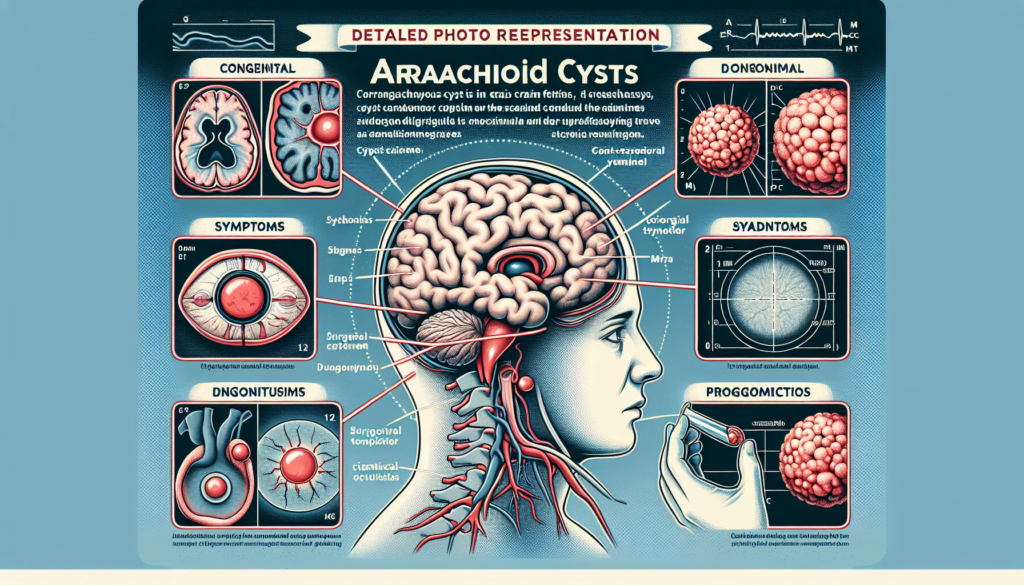
Understanding Arachnoid Cysts
Definition and Composition
Arachnoid cysts are defined as collections of cerebrospinal fluid (CSF) that arise from the splitting layers of the arachnoid membrane, one of the three meningeal layers that cover the brain and spinal cord. These cysts are typically covered by arachnoidal cells and collagen, and they may develop between the surface of the brain and the cranial base or directly on the arachnoid membrane. Arachnoid cysts can be found both in the brain and on the spine, where they are categorized based on their specific location and the type of fluid they contain.
Classification of Arachnoid Cysts
Arachnoid cysts can be broadly classified into two main types: primary and secondary. Primary arachnoid cysts are congenital, meaning they are present at birth and often result from developmental abnormalities during the early weeks of gestation. These cysts are commonly found in specific areas such as the middle cranial fossa and the Sylvian fissure.
Secondary arachnoid cysts, on the other hand, develop due to external factors such as head injury, meningitis, tumors, or as a complication following brain surgery. These cysts are less common than primary cysts and may appear in various locations depending on the underlying cause.
For more detailed classification, the Galassi classification system is widely used, particularly for cysts located in the middle cranial fossa. This system categorizes the cysts into three types based on their size and the degree of displacement of adjacent brain structures:
- Type I cysts are small and usually asymptomatic, confined to the anterior portion of the middle cranial fossa.
- Type II cysts are larger, extend along the Sylvian fissure, and may displace the temporal lobe.
- Type III cysts are the largest, occupying the entire middle cranial fossa and causing displacement of the temporal, parietal, and frontal lobes.
These classifications help in determining the potential impact of the cysts on surrounding brain structures and are crucial in guiding treatment decisions.
Causes and Risk Factors
Congenital Causes
Arachnoid cysts are frequently congenital, appearing primarily at birth. These are often termed primary arachnoid cysts and arise due to the abnormal growth of the arachnoid membrane during fetal development. The exact mechanism behind the formation of these cysts remains unclear, but it is suggested that a split in the arachnoid membrane, which is one of the three layers of tissue that surround and protect the brain and spinal cord, plays a crucial role. Some evidence points to a genetic predisposition for these cysts, indicating that they can occasionally run in families, although this is rare.
Secondary Causes
Secondary arachnoid cysts, also known as noncongenital arachnoid cysts, develop due to external factors rather than being present at birth. These can result from head injuries, complications from brain or spinal surgery, infections like meningitis, or the presence of brain tumors. These factors can lead to the direct irritation of the arachnoid matter by inflammatory mediators, either endogenous from blood products or exogenous endotoxins from bacterial infections. This irritation can cause adhesive arachnoiditis, which is a condition where the arachnoid layer of the meninges becomes inflamed and sticky, leading to the accumulation of cerebrospinal fluid (CSF) through a slit-valve mechanism. Over time, this can result in increased cyst size and potentially marked increases in intracranial pressure. Additionally, surgical manipulations and the presence of blood in the subarachnoid space have been hypothesized to trigger an inflammatory process in the arachnoid membranes, further contributing to cyst formation.
Symptoms of Arachnoid Cysts
Common Symptoms
Arachnoid cysts are often asymptomatic, but when symptoms occur, they typically manifest before the age of 20, especially during the first year of life. The symptoms range from mild to severe, depending on the cyst’s size, location, and whether it is exerting pressure on nerves, the brain, or the spinal cord. Common symptoms include:
- Headaches
- Nausea and vomiting
- Seizures
- Hydrocephalus, characterized by an excess accumulation of cerebrospinal fluid in the brain
- Vertigo and dizziness
- Lethargy, which includes excessive fatigue or low energy
- Visible lumps or protrusions from the head or spine
Symptoms Based on Location
The location of an arachnoid cyst significantly influences the specific symptoms experienced by individuals. Here are symptoms associated with cysts in various regions:
- Middle Fossa Region: Cysts in this area can disrupt vision, hearing, movement, and balance. They may cause fatigue and weakness or paralysis, typically on one side of the body. In children, these cysts might lead to developmental delays and behavioral changes.
- Suprasellar Region: These cysts can impair vision and affect the endocrine system, which controls processes like puberty and sexual development. Some individuals experience involuntary head bobbing, moving their heads side to side or in a circular motion, reminiscent of a bobble-head doll.
- Spinal Cord: Spinal arachnoid cysts may cause numbness and tingling in the feet and hands, muscle spasms, movement issues, and paralysis. Common additional symptoms include back pain and scoliosis. In some cases, these cysts lead to urinary tract infections.
- Other Locations: Cysts in less common areas might lead to more severe symptoms due to mass effect or cyst rupture. Symptoms can include vision loss, macrocephaly, paralysis of cranial nerves, trigeminal neuropathy, hemifacial spasm, sensory neuronal hearing loss, facial palsy, vertigo, and eighth cranial neuropathy. Rarely, symptoms like learning difficulties and attention deficit hyperactivity disorder are noted, particularly with temporal arachnoid cysts.
Overall, the symptoms of arachnoid cysts are diverse and heavily dependent on the cyst’s location within the cranial or spinal regions.
Diagnosis of Arachnoid Cysts
Imaging Techniques
The diagnosis of arachnoid cysts primarily relies on imaging techniques, with Magnetic Resonance Imaging (MRI) being the diagnostic procedure of choice. MRI is instrumental due to its ability to precisely demonstrate the location, size, and relationship of the cysts to the brain and spinal cord. On MRI scans, arachnoid cysts appear as well-defined, nonenhancing masses that are isointense to cerebrospinal fluid (CSF) across various sequences. These include T1-weighted, T2-weighted, and Fluid-Attenuated Inversion Recovery (FLAIR) sequences. Importantly, arachnoid cysts maintain CSF signal characteristics on all these sequences, which is crucial for their identification.
Diffusion Weighted Imaging (DWI) is another critical MRI technique used in the diagnosis. While most arachnoid cysts show signal loss on DWI, those containing proteinaceous fluid or blood may not, which can sometimes lead to diagnostic challenges. Furthermore, MRI cisternography, which can be performed with or without contrast, helps in visualizing the cyst’s connection to the surrounding CSF space. Advanced MRI techniques such as Constructive Interference in Steady State (CISS), Fast Imaging Employing Steady-State Acquisition (FIESTA), and 3D T2-weighted Sampling Perfection with Application-optimized Contrasts using different flip-angle Evolutions (3D SPACE) are particularly useful for detailed visualization of the cyst wall and adjacent structures.
Computed Tomography (CT) imaging, while less detailed, can still effectively diagnose most arachnoid cysts, especially when they are fluid-filled and thin-walled. CT cisternography, which involves the injection of a contrast medium into the subarachnoid space, can also be employed to assess the communication of the cyst with the CSF space, providing valuable information for management decisions.
Differential Diagnosis
The differential diagnosis for arachnoid cysts includes several other types of cysts and mass lesions, which can appear similar on imaging studies. Epidermoid cysts, for instance, share imaging characteristics with arachnoid cysts on T1-weighted and T2-weighted MRI but can be distinguished by their elevated signals on diffusion-weighted imaging and their lack of enhancement with gadolinium. Dermoid cysts and lipomas can be identified by their signal intensities that follow fat, which can be confirmed using T1 sequences with and without fat saturation.
Other differential considerations include abscesses, which typically present with rim enhancement and a central fluid signal that differs from CSF due to inflammatory debris. Neurocysticercosis, a parasitic infection, might also mimic arachnoid cysts but usually presents with additional signs like calcifications and a multiloculated appearance. Pineal cysts, glial cysts, Rathke’s cleft cysts, and colloid cysts are also part of the differential diagnosis, each with distinct imaging features that help in their identification and differentiation from arachnoid cysts.
This comprehensive approach using various imaging techniques and understanding the differential diagnosis is essential for accurate identification and management of arachnoid cysts.
Treatment Options
Non-Surgical Treatments
Arachnoid cysts that are discovered incidentally and remain asymptomatic generally do not require immediate treatment. The primary management strategy for these cysts is regular monitoring through serial imaging or MRI scans to detect any changes in size or new symptoms that may arise. This approach allows healthcare providers to recommend further intervention if the cyst begins to produce problems over time.
Surgical Interventions
When arachnoid cysts become symptomatic, surgical intervention is often necessary to alleviate the symptoms and prevent potential complications such as neurological damage. The choice of surgical technique is influenced by the cyst’s size, location, and the specific symptoms it causes.
- Shunt Placement: A common surgical method involves the installation of a cysto-peritoneal shunt. This procedure diverts the fluid from the cyst into the abdominal cavity, where it can be absorbed naturally by the body. Shunting is particularly used for recurrent cysts and is considered a last resort in some cases due to the potential risks of shunt failure.
- Craniotomy Fenestration: This technique requires opening the skull to access and open the cyst, allowing the fluid to drain into the basal CSF cisterns. Craniotomy fenestration aims to create a permanent solution by making the cyst communicate with other fluid spaces in the brain.
- Endoscopic Cyst Fenestration: As a minimally invasive alternative, endoscopic cyst fenestration involves using an endoscope to internally drain the cyst. This method combines the benefits of direct cyst drainage with a reduced risk of complications associated with more invasive procedures. The procedure is quick, typically taking between 30 minutes to an hour, and patients can often return home the following day.
The selection of a surgical approach also depends on the cyst’s location. For example, cysts in the suprasellar and quadrigeminal regions are often treated effectively with neuroendoscopy, while interhemispheric cysts might require microsurgical fenestration. Each surgical option is planned based on detailed preoperative imaging, which helps in identifying the optimal trajectory and site for fenestration, ensuring a high success rate and minimizing risks.
In conclusion, the treatment of arachnoid cysts varies widely, ranging from watchful waiting in asymptomatic cases to various surgical interventions in symptomatic cases. The decision on the most appropriate treatment method takes into account the cyst’s characteristics, associated symptoms, and potential risks involved with each procedure.
Prognosis and Complications
Long-term Outlook
The long-term outlook for individuals with arachnoid cysts varies significantly based on the cyst’s size, location, and whether symptoms are present. Many arachnoid cysts remain stable and asymptomatic throughout an individual’s life, requiring no treatment. Regular monitoring through imaging is often sufficient for these cases.
For symptomatic arachnoid cysts, the prognosis after surgical intervention is generally favorable. Most individuals experience relief from symptoms and a significant improvement in quality of life post-surgery. The success of surgical outcomes largely depends on the precise execution of the procedure and the cyst’s response to surgical intervention.
Potential Complications
While many arachnoid cysts are benign and do not lead to serious complications, they can pose significant risks if they begin to grow or cause pressure effects on surrounding structures. Some of the potential complications associated with arachnoid cysts include:
- Neurological Impairment: Large cysts may exert pressure on adjacent brain or spinal cord structures, potentially leading to weakness, sensory loss, or coordination problems.
- Hydrocephalus: If a cyst blocks the flow of cerebrospinal fluid (CSF), it can lead to an accumulation of fluid in the brain, a condition known as hydrocephalus. This can increase intracranial pressure and require urgent medical intervention.
- Hemorrhage: Although rare, arachnoid cysts can bleed internally, especially if they are located near blood vessels. This can lead to sudden, severe symptoms and necessitate emergency treatment.
- Cyst Rupture: A ruptured arachnoid cyst can release fluid into surrounding areas, leading to potential irritation and inflammation of nearby tissues.
Monitoring for these complications is crucial, especially in individuals with known risk factors or larger cysts. Regular follow-up imaging helps in early detection of changes in cyst size or effects on surrounding tissues, allowing timely medical or surgical intervention.
Conclusion
Through the expansive outline provided, it’s evident that arachnoid cysts, while often asymptomatic, pose a complex challenge when they become symptomatic, affecting individuals’ health in diverse and sometimes significant ways. The article extensively covered the nature of these cysts—from their classification, causes, and symptoms, to diagnostic procedures and treatment options—highlighting the strides made in medical science for their management. The exploration of potential complications and the prognosis for those affected offers a comprehensive understanding, aiming to equip readers with the knowledge needed to navigate this health issue effectively.
The significance of this discussion extends beyond the immediate concerns of diagnosis and treatment, underscoring the importance of continued research and patient education in the field of neurology. By fostering informed conversations between patients and healthcare providers, individuals can make educated decisions regarding their care. Further research may unveil more about the causes and long-term management of arachnoid cysts, potentially leading to innovative treatment methods and improved outcomes for those living with this condition.