Autoimmune hepatitis is a rare but serious condition that affects the liver. This chronic disease occurs when the body’s immune system mistakenly attacks healthy liver cells, causing inflammation and damage. Understanding autoimmune hepatitis is crucial for those affected by it, as early diagnosis and proper treatment can help manage symptoms and prevent long-term complications.
This article delves into the key aspects of autoimmune hepatitis, providing valuable insights for patients and caregivers alike. It explores the symptoms to watch out for, sheds light on potential causes and risk factors, and discusses the diagnostic process. Additionally, it examines current treatment options available to help control the disease and improve quality of life for those living with autoimmune hepatitis.
What is Autoimmune Hepatitis?
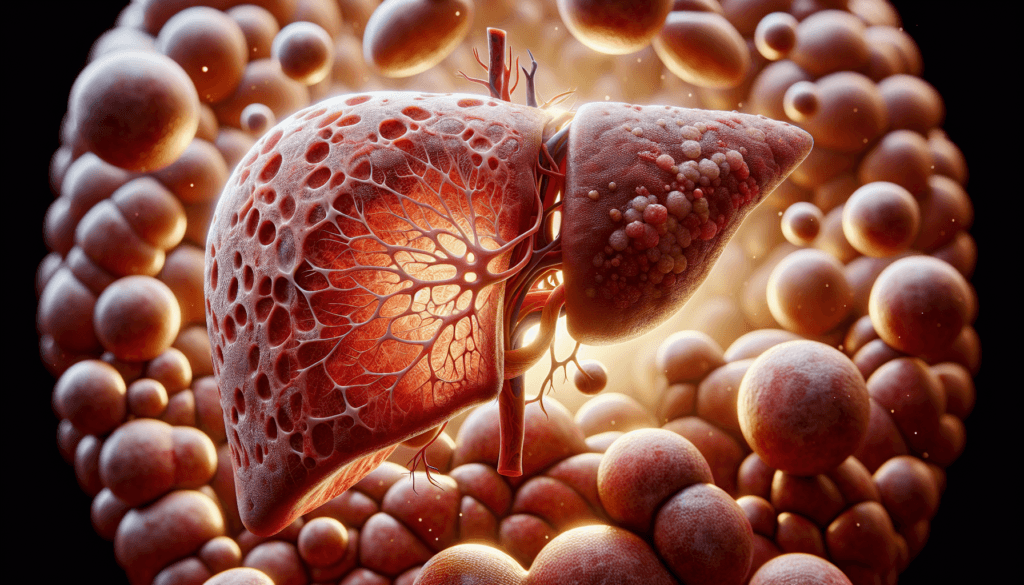
Autoimmune hepatitis is a chronic disease in which the body’s immune system mistakenly attacks the liver cells, causing inflammation and damage. The exact cause of this condition remains unknown, but it is believed to result from a complex interplay of genetic predisposition, environmental triggers, and immune system dysfunction.
Definition
Autoimmune hepatitis is characterized by the presence of specific autoantibodies that target liver cells, leading to persistent inflammation and progressive liver damage. If left untreated, this condition can lead to cirrhosis, liver failure, and other serious complications.
RELATED: Polycythemia Vera: From Diagnosis to Treatment – A Complete Guide
Types of AIH
There are two main types of autoimmune hepatitis: Type 1 and Type 2. Type 1 AIH is the most common form, accounting for approximately 80% of cases. It is distinguished by the presence of anti-smooth muscle antibodies (ASMA) and/or antinuclear antibodies (ANA). Type 2 AIH is less common and is characterized by the presence of anti-liver/kidney microsome type 1 (anti-LKM1) antibodies or anti-liver cytosol type 1 (anti-LC1) antibodies. Type 2 AIH tends to affect children and young adults more frequently than Type 1.
Prevalence
The exact prevalence of autoimmune hepatitis is difficult to determine, as the condition may go undiagnosed in many cases. However, studies suggest that the global pooled incidence of AIH is approximately 1.28 cases per 100,000 inhabitant-years, while the prevalence is estimated to be around 15.65 cases per 100,000 inhabitants. In the United States, a recent population-based study found the prevalence of AIH to be 31.2 cases per 100,000 individuals between 2014 and 2019. The disease is more common in females, with a female-to-male ratio of approximately 3.6:1. Additionally, AIH can affect individuals of all ages and ethnicities, although it is more frequently diagnosed in adults and Caucasians.
Symptoms and Signs
Common symptoms
The symptoms of autoimmune hepatitis can vary widely, with some individuals experiencing no symptoms at all while others develop severe liver disease. Common symptoms include fatigue, abdominal discomfort, joint pain, and skin rashes. In more advanced cases, patients may experience jaundice, dark urine, pale stools, and itching due to the buildup of bile in the bloodstream. Nausea, loss of appetite, and weight loss are also frequently reported.
Advanced symptoms
As autoimmune hepatitis progresses and liver function deteriorates, additional symptoms may emerge. These include spider angiomas, enlarged veins in the esophagus (varices), easy bruising and bleeding, loss of menstrual periods in women, and fluid accumulation in the abdomen (ascites) or hands and feet (edema). In severe cases, confusion, disorientation, or drowsiness (hepatic encephalopathy) can occur due to the liver’s inability to remove toxins from the blood effectively.
RELATED: Poison Hemlock: Detailed Guide on Identification and Control
Asymptomatic cases
It is important to note that not everyone with autoimmune hepatitis experiences symptoms, especially in the early stages of the disease. In some cases, the condition is discovered incidentally during routine blood tests that reveal elevated liver enzymes. This highlights the importance of regular check-ups and liver function monitoring, particularly for individuals with a family history of autoimmune diseases or other risk factors for autoimmune hepatitis. Early detection and intervention can help prevent the progression of liver damage and improve long-term outcomes for patients with this chronic condition.
Causes and Risk Factors
Genetic factors
While the exact cause of autoimmune hepatitis remains unknown, a complex interplay between genetic predisposition, environmental triggers, and immune system dysfunction is believed to contribute to its development. Genetic studies have identified certain human leukocyte antigen (HLA) alleles that are associated with an increased risk of developing AIH. In European populations, the HLA-DRB103:01 and HLA-DRB104:01 alleles have been strongly linked to AIH susceptibility. However, the predisposing HLA alleles vary among different ethnicities and geographic regions. For instance, HLA-DRB104:05 and HLA-DRB104:04 are associated with AIH in Latin American populations, while HLA-DRB104:05 and HLA-DRB104:01 are linked to the disease in Japanese individuals.
Environmental triggers
Environmental factors, such as viral infections, drugs, and toxins, are thought to play a crucial role in triggering the autoimmune response in genetically susceptible individuals. Viral infections, including hepatitis A, B, C, D, and E viruses, as well as Epstein-Barr virus, cytomegalovirus, and herpes simplex virus type 1, have been associated with the development of AIH. These viruses may induce molecular mimicry, where the immune system mistakenly attacks liver cells due to similarities between viral and liver antigens. Additionally, certain medications, such as nitrofurantoin and minocycline, have been implicated in drug-induced AIH. Exposure to environmental toxins and xenobiotics may also contribute to the development of AIH by generating neoantigens or modifying liver proteins, rendering them immunogenic.
Associated conditions
Autoimmune hepatitis is often associated with other autoimmune disorders, suggesting a shared genetic predisposition or common pathogenic mechanisms. Patients with AIH have an increased risk of developing concurrent autoimmune diseases, such as autoimmune thyroiditis, rheumatoid arthritis, celiac disease, and ulcerative colitis. The presence of these associated conditions can influence the clinical presentation, disease course, and treatment response in individuals with AIH. Regular screening for comorbid autoimmune diseases is essential for the comprehensive management of patients with autoimmune hepatitis.
Diagnosis and Treatment
Diagnostic tests
Diagnosing autoimmune hepatitis requires a combination of medical history, physical examination, laboratory tests, and liver biopsy. Blood tests play a crucial role in the diagnostic process, including liver function tests to assess transaminase levels (AST and ALT) and gamma globulin concentrations. Elevated IgG levels are also a common finding in autoimmune hepatitis. Autoantibody tests, such as antinuclear antibodies (ANA), smooth muscle antibodies (SMA), and liver-kidney microsomal type 1 (anti-LKM1) antibodies, are essential for diagnosis and subtype classification. Other autoantibodies, like anti-soluble liver antigen (anti-SLA) and anti-liver cytosol type 1 (anti-LC1), may also be present. Imaging studies, such as ultrasound, CT, or MRI, can help evaluate liver size, shape, and texture, as well as exclude other causes of liver disease. However, liver biopsy remains the gold standard for confirming the diagnosis, assessing the severity of inflammation and fibrosis, and guiding treatment decisions.
RELATED: Pheochromocytoma: Detailed Overview of Symptoms and Treatments
Treatment options
The primary goal of treatment in autoimmune hepatitis is to achieve remission, prevent disease progression, and improve long-term survival. Corticosteroids, particularly prednisone, are the mainstay of therapy. Treatment typically begins with a high dose of prednisone (30-60 mg/day) and is gradually tapered over several weeks to a maintenance dose of 10-20 mg/day. Azathioprine, an immunosuppressant, is often used in combination with prednisone to minimize steroid-related side effects and maintain remission. In cases of intolerance or incomplete response to standard therapy, alternative immunosuppressants, such as mycophenolate mofetil, cyclosporine, or tacrolimus, may be considered. Treatment duration varies but usually lasts for at least 18-24 months, with regular monitoring of liver function tests and autoantibody levels. Relapse is common after treatment discontinuation, and some patients may require lifelong maintenance therapy.
Prognosis
The prognosis of autoimmune hepatitis largely depends on the timely diagnosis and initiation of appropriate treatment. With proper management, most patients achieve remission and have a favorable long-term outcome. However, untreated or inadequately treated autoimmune hepatitis can lead to progressive liver damage, cirrhosis, and ultimately liver failure. Patients who develop cirrhosis are at increased risk of complications, such as portal hypertension, esophageal varices, and hepatocellular carcinoma. In cases of acute liver failure or end-stage liver disease, liver transplantation may be necessary. Close monitoring, adherence to treatment, and regular follow-up with a hepatologist are essential for optimizing outcomes in patients with autoimmune hepatitis.
Conclusion
Autoimmune hepatitis is a complex condition that has a significant impact on liver health and overall well-being. Early detection and proper treatment play a crucial role in managing the disease and preventing long-term complications. By understanding the symptoms, causes, and available treatment options, patients and healthcare providers can work together to develop effective management strategies and improve outcomes.
While living with autoimmune hepatitis can be challenging, ongoing research and advancements in medical care offer hope for better treatments and improved quality of life. Regular check-ups, adherence to prescribed therapies, and a healthy lifestyle are key to keeping the condition in check. With the right approach and support, many individuals with autoimmune hepatitis can lead fulfilling lives and keep their liver health in good shape.