Diverticulitis is a painful and often misunderstood digestive condition that affects millions of people worldwide. While it is more common in older adults, diverticulitis can strike at any age, causing a range of uncomfortable symptoms and potentially serious complications. Understanding the causes, symptoms, and treatment options for diverticulitis is crucial for those who suffer from this condition or are at risk of developing it.
In this comprehensive guide, we will delve into the details of diverticulitis, exploring what it is and how it develops. We will discuss the various symptoms associated with diverticulitis, helping you recognize when to seek medical attention. Additionally, we will examine the underlying causes and risk factors, as well as the diagnostic tests used to confirm the presence of the condition. Furthermore, we will outline the available treatment options, including dietary modifications, medications, and surgical interventions, and provide insights into preventing future episodes through lifestyle changes.
What is Diverticulitis?
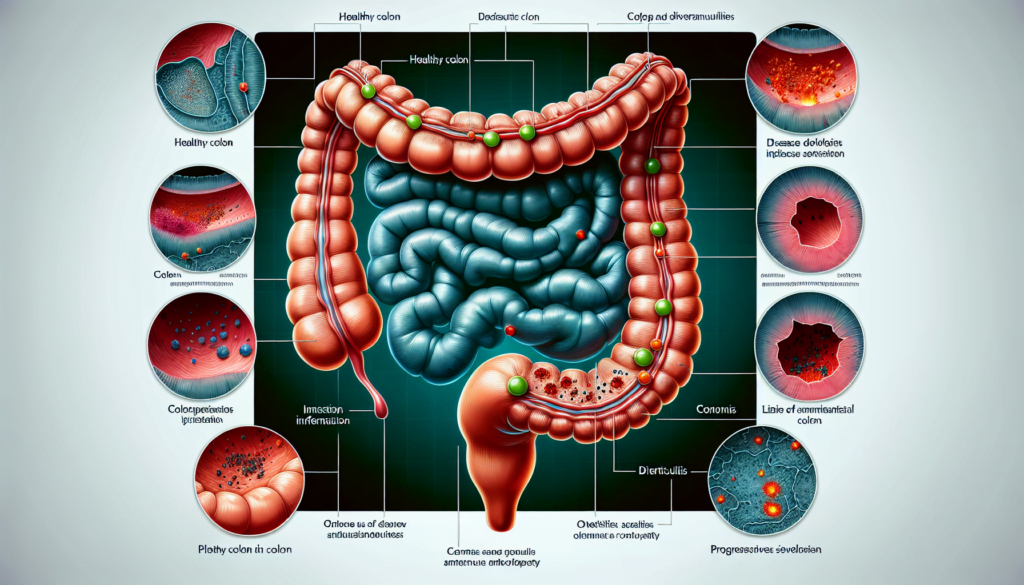
Diverticulitis is a condition that occurs when small, bulging pouches called diverticula, which form in the digestive tract, become inflamed or infected. These pouches typically develop in the lower part of the large intestine, known as the sigmoid colon. While the presence of diverticula alone is called diverticulosis and is relatively common, especially in older adults, diverticulitis specifically refers to the inflammation of one or more of these pouches.
The wall of the colon is usually smooth, but when diverticula form, they create irregular bulges. Diverticula are common, particularly after the age of 50, and most often do not cause any problems. However, when these pouches become inflamed, the condition is then referred to as diverticulitis.
Inflammation in diverticulitis is a result of the body’s immune system response, which increases blood flow and fluid delivery to the affected area, along with disease-fighting cells. This inflammation can lead to a range of symptoms, including severe pain, fever, nausea, and changes in bowel habits.
The severity of diverticulitis can vary, with mild cases often treated with rest, dietary changes, and possibly antibiotics, while more severe cases may require hospitalization and intravenous antibiotic treatment. In some instances, surgery may be necessary to address complications or recurrent episodes of diverticulitis.
Symptoms of Diverticulitis
The symptoms of diverticulitis can range from mild to severe, often starting suddenly and worsening over a few days. A common symptom is pain in the lower left abdomen, which is usually sudden and intense. The pain may be constant or vary in intensity over time.
Other signs and symptoms of diverticulitis may include:
- Nausea
- Fever
- Tenderness in the abdomen when touched
- Changes in stool, including sudden diarrhea or constipation
People with diverticulosis, the condition where small pouches called diverticula form in the digestive tract, often have no symptoms. However, they may experience bloating and cramping in the lower part of the belly. In rare cases, they may notice blood in their stool or on toilet paper.
When one or more diverticula become inflamed or infected, the condition is called diverticulitis. Symptoms of diverticulitis are more severe compared to diverticulosis and often start abruptly. These symptoms include:
- Tenderness, usually in the left lower part of the abdomen
- Bloating or gas
- Fever and chills
- Nausea and vomiting
- Loss of appetite
It is essential to seek medical care if you experience constant, unexplained abdominal pain, particularly if it is accompanied by a fever and notable changes in bowel habits. Early diagnosis and treatment can help manage the symptoms and prevent complications associated with diverticulitis.
Causes and Risk Factors
Several factors can contribute to the development of diverticulitis and increase the risk of experiencing this condition. While the exact causes are not fully understood, a combination of genetic, lifestyle, and other factors are believed to play a role.
Diverticula, the small pouches that form in the colon wall, develop gradually over time and are more common in older adults. Pressure within the colon, possibly from spasms or straining, may cause these pouches to form in areas where the colon wall is weak. Diverticulitis occurs when one or more diverticula become inflamed, which can happen due to bacterial infection or damage to the diverticular tissues.
Some of the key risk factors for developing diverticulitis include:
- Age: The likelihood of developing diverticulitis increases with age, particularly after the age of 50.
- Obesity: Being overweight or obese is associated with a higher risk of diverticulitis.
- Smoking: Cigarette smoking has been linked to an increased risk of developing diverticular disease and its complications.
- Diet: A diet low in fiber and high in red meat may increase the risk of diverticulitis. Consuming adequate fiber helps maintain regular bowel movements and reduces pressure within the colon.
- Lack of exercise: Leading a sedentary lifestyle with minimal physical activity can increase the risk of diverticular disease.
- Certain medications: The use of steroids, opioids, and non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen sodium has been associated with a higher risk of diverticulitis.
- Vitamin D deficiency: Low levels of vitamin D in the body have been linked to an increased risk of diverticulitis.
In addition to these risk factors, research suggests that genetics may also play a role in the development of diverticular disease. Certain genes may make some individuals more susceptible to developing diverticula.
Other factors currently being studied for their potential role in diverticular disease include:
- Bacteria or stool becoming trapped in the diverticula
- Changes in the gut microbiome
- Issues with connective tissue, muscles, or nerves in the colon
- Immune system dysfunction
By understanding the causes and risk factors associated with diverticulitis, individuals can take steps to modify their lifestyle and reduce their likelihood of developing this condition. Maintaining a healthy diet rich in fiber, exercising regularly, maintaining a healthy weight, and avoiding smoking and excessive alcohol consumption can help lower the risk of diverticulitis and its complications.
Diagnosis and Tests
To diagnose diverticulitis, doctors typically start by reviewing the patient’s medical history and conducting a physical examination. They may ask about symptoms, bowel movement patterns, diet, medical conditions, and medications. During the physical exam, the doctor checks for tenderness or masses in the abdomen, listens to abdominal sounds with a stethoscope, and may perform a digital rectal exam.
Several tests can help confirm the diagnosis of diverticulitis and rule out other conditions:
- Blood Tests: Blood samples are analyzed to check for signs of infection, such as an elevated white blood cell count, which is common in diverticulitis.
- Stool Test: A stool sample may be collected to rule out other conditions that cause similar symptoms, such as irritable bowel syndrome or inflammatory bowel disease.
- Imaging Tests: Computed tomography (CT) scans, ultrasounds, or magnetic resonance imaging (MRI) can provide detailed images of the colon, revealing inflamed or infected diverticula, abscesses, or other complications.
- Colonoscopy: In some cases, a colonoscopy may be recommended to confirm the diagnosis and rule out other conditions like colon cancer. During this procedure, a long, flexible tube with a camera on the end is inserted into the rectum and guided through the colon, allowing the doctor to visually examine the lining of the intestine.
If diverticula are discovered incidentally during tests performed for other reasons, and there are no associated symptoms, the condition is diagnosed as diverticulosis rather than diverticulitis.
Prompt and accurate diagnosis of diverticulitis is essential for initiating appropriate treatment and preventing potential complications. By combining information from the patient’s history, physical examination, and diagnostic tests, doctors can effectively diagnose diverticulitis and develop an individualized treatment plan.
Treatment Options
The treatment options for diverticulitis depend on the severity of the condition and the individual’s overall health. Treatment may include home remedies, medications, and in some cases, surgical intervention.
Home Remedies
During a mild episode of diverticulitis, doctors may recommend a clear liquid diet for a few days to help rest the colon and allow inflammation to subside. This diet includes:
- Water, tea, and coffee without milk or cream
- Broth
- Ice pops without fruit pieces or pulp
- Gelatin
- Clear fruit juices without pulp
As symptoms improve, a low-fiber diet can be gradually introduced. Applying a heating pad to the abdomen may also provide relief from mild cramps and pain.
Medications
Antibiotics are often prescribed to treat acute diverticulitis, especially if there is a risk of complications such as abscess formation or perforation. Common antibiotics used include:
- Amoxicillin/clavulanic acid
- Sulfamethoxazole
Pain management is another important aspect of treatment. Acetaminophen and antispasmodics may be recommended for pain relief. However, nonsteroidal anti-inflammatory drugs (NSAIDs) should be avoided as they may increase the risk of complications.
For persistent symptoms after an acute episode, a low-dose tricyclic antidepressant, such as nortriptyline, may be prescribed to help manage abdominal pain.
Surgical Treatments
Surgery is typically reserved for severe cases of diverticulitis or when complications arise. Indications for surgery include:
- Recurrent episodes of uncomplicated diverticulitis
- Perforation of the colon
- Abscess formation not responsive to antibiotics
- Fistula formation
- Intestinal obstruction or stricture
The most common surgical procedure is a sigmoid resection (sigmoidectomy), where the affected portion of the colon is removed, and the remaining ends are reconnected. This can be performed through an open incision or laparoscopically, depending on the situation and the surgeon’s preference.
In cases of severe complications, such as peritonitis or uncontrolled bleeding, emergency surgery may be necessary. A temporary colostomy may be required to allow the colon to heal before a second surgery is performed to reconnect the bowel.
Elective surgery may be considered for individuals with recurrent episodes of diverticulitis or chronic symptoms that significantly impact their quality of life. The decision to proceed with surgery should be made on a case-by-case basis, considering the potential benefits and risks.
In summary, the treatment of diverticulitis involves a combination of dietary modifications, antibiotics, pain management, and in severe or recurrent cases, surgical intervention. Working closely with a healthcare provider is essential to develop an individualized treatment plan based on the severity of the condition and the patient’s overall health.
Complications to Watch for
While most cases of diverticulitis are uncomplicated and respond well to treatment, approximately 15% of patients with diverticulitis symptoms may experience complications. These complications can range from mild to severe and may require prompt medical attention.
Some of the potential complications associated with diverticulitis include:
- Abscess formation: In up to 30% of cases, diverticulitis can lead to the development of an abscess, which is a localized collection of pus. Abscesses typically manifest as hypoechoic fluid collections with thick walls on ultrasound and as hypodense fluid-attenuated lesions with intensely enhancing walls on CT.
- Perforation: Severe inflammation in diverticulitis can cause perforation of the colon wall, allowing intestinal contents to leak into the abdominal cavity. This can lead to peritonitis, a serious condition that requires immediate medical intervention. CT findings of perforation include extraluminal gas, focal bowel wall discontinuity, and extraluminal contrast leakage.
- Fistula formation: Approximately 14% of patients with acute diverticulitis may develop fistulas, which are abnormal connections between the colon and nearby organs or structures. The most common types of fistulas are colovesical (between the colon and bladder), coloenteric (between the colon and small intestine), and colouterine (between the colon and uterus). CT may demonstrate air within the bladder or uterine cavity, suggesting the presence of a fistula.
- Intestinal obstruction: Chronic inflammation and fibrosis associated with recurrent diverticulitis can lead to partial or complete bowel obstruction. This complication is characterized by irregular wall thickening and upstream bowel dilatation on imaging studies.
- Pylephlebitis: Also known as septic thrombophlebitis, pylephlebitis is a rare but serious complication of diverticulitis. It involves the development of septic thrombi in the mesenteric and portal venous system, which can lead to liver abscesses and septic pulmonary emboli. Contrast-enhanced CT is the modality of choice for diagnosing pylephlebitis, demonstrating endoluminal thrombi as filling defects in the affected veins.
- Bleeding: Although less common than previously thought, bleeding can occur in approximately 5% of patients with diverticulitis. Contrast-enhanced CT performed in the arterial phase may demonstrate active extravascular contrast extravasation into the diverticulum and bowel lumen.
Prompt recognition and appropriate management of these complications are crucial to prevent increased morbidity and mortality. Radiologists play a vital role in identifying these complications using various imaging modalities, such as ultrasonography and computed tomography. A thorough understanding of the imaging features associated with each complication is essential for accurate diagnosis and guiding appropriate treatment decisions.
Prevention and Lifestyle Modifications
While there is no guaranteed way to prevent diverticulitis, making certain lifestyle changes can significantly reduce the risk of developing this condition and experiencing its painful symptoms. Incorporating the following modifications into your daily routine may help keep your digestive system healthy and minimize the likelihood of diverticulitis flare-ups:
- Eat a high-fiber diet: Gradually increase your intake of fiber-rich foods, such as whole grains, fruits, vegetables, and legumes. Fiber helps to soften stool and promote regular bowel movements, reducing the pressure within the colon that can lead to the formation of diverticula. Aim for 25-35 grams of fiber per day, but be sure to increase your intake slowly to avoid bloating and gas.
- Stay hydrated: Drink plenty of water and other fluids throughout the day to help keep stools soft and prevent constipation. Adequate hydration is especially important when increasing your fiber intake, as fiber absorbs water to add bulk to the stool.
- Exercise regularly: Engaging in physical activity helps to promote regular bowel movements and maintain a healthy weight. Aim for at least 30 minutes of moderate exercise, such as brisk walking or cycling, most days of the week.
- Maintain a healthy weight: Being overweight or obese increases the risk of developing diverticulitis. Adopting a balanced diet and regular exercise routine can help you achieve and maintain a healthy weight, reducing the strain on your digestive system.
- Limit red meat consumption: Some studies suggest that a diet high in red meat may increase the risk of diverticulitis. Consider reducing your intake of red meat and replacing it with lean protein sources, such as poultry, fish, and plant-based options like legumes and tofu.
- Quit smoking: Smoking has been linked to an increased risk of diverticulitis and its complications. If you currently smoke, consider quitting to improve your overall health and reduce your risk of developing diverticular disease.
- Manage stress: While the connection between stress and diverticulitis is not fully understood, managing stress through techniques like meditation, deep breathing exercises, or yoga may contribute to better overall digestive health.
- Consider probiotics: Probiotics are beneficial bacteria that can help maintain a healthy balance of gut flora. Some research suggests that consuming probiotic-rich foods, such as yogurt or kefir, or taking probiotic supplements may help prevent diverticulitis, although more studies are needed to confirm this.
By making these lifestyle modifications, you can take proactive steps towards preventing diverticulitis and promoting better digestive health. Remember to consult with your healthcare provider before making significant changes to your diet or starting a new exercise routine, especially if you have pre-existing medical conditions.
Conclusion
Understanding diverticulitis is crucial for those who suffer from this condition or are at risk of developing it. By recognizing the symptoms, causes, and available treatment options, individuals can take proactive steps to manage their digestive health and prevent potential complications. Making lifestyle modifications, such as adopting a high-fiber diet, staying hydrated, exercising regularly, and managing stress, can significantly reduce the risk of developing diverticulitis.
If you suspect that you may have diverticulitis, it is essential to seek medical attention promptly. Early diagnosis and appropriate treatment can help alleviate symptoms, prevent complications, and improve overall quality of life. By working closely with your healthcare provider and making necessary lifestyle changes, you can effectively manage diverticulitis and maintain optimal digestive health.