Kidney failure is a serious medical condition that affects millions of people worldwide. When the kidneys stop functioning properly, it can have a profound impact on overall health and quality of life. Understanding kidney failure, its symptoms, and available treatments is crucial for those at risk or already diagnosed with this condition.
This comprehensive guide aims to shed light on the complexities of kidney failure. It will explore the essential functions of healthy kidneys, discuss different types of kidney failure, and outline common symptoms to watch for. Additionally, the article will delve into diagnosis methods and various treatment options available to manage kidney failure effectively. By providing this information, readers can gain valuable insights to better understand and address this challenging health issue.
Understanding Kidney Function
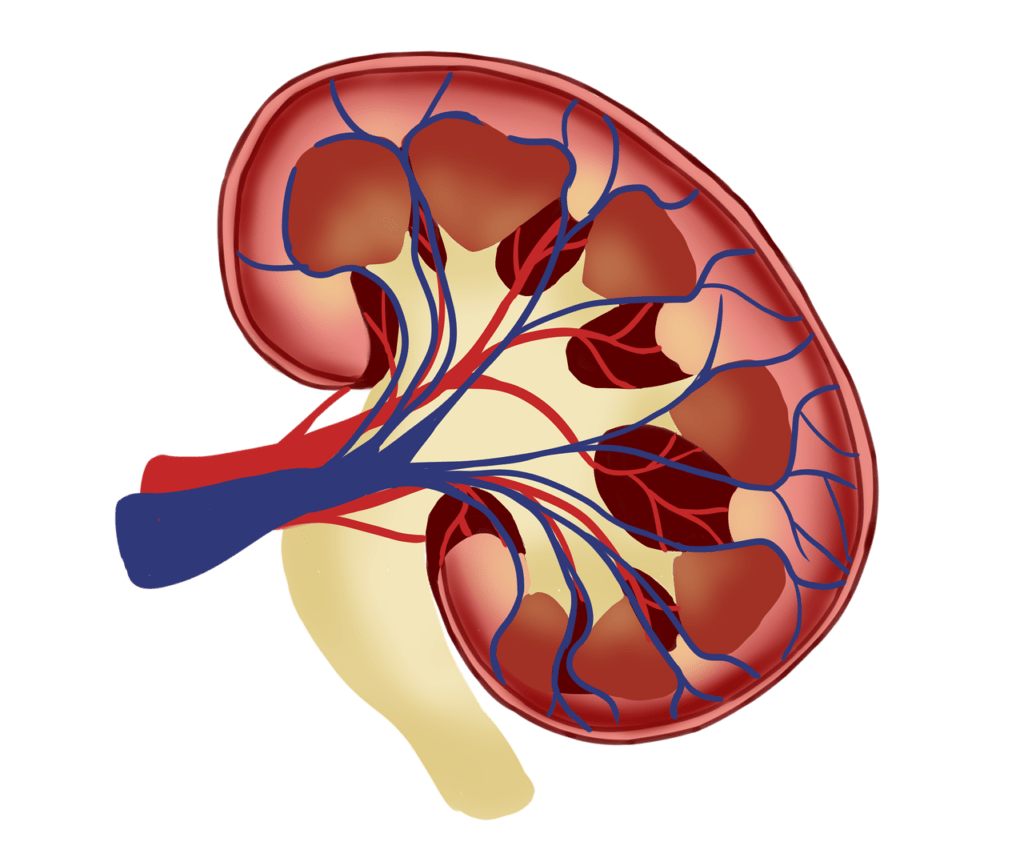
The kidneys, two bean-shaped organs located on either side of the spine just below the rib cage, play a vital role in maintaining overall health and well-being. These powerful chemical factories perform a variety of essential functions that keep the body functioning properly.
Role of kidneys in the body
One of the primary roles of the kidneys is to filter waste products and excess fluid from the blood. Each kidney contains up to 1.5 million tiny tubes called nephrons, which act as the body’s filtration system. As blood flows through the nephrons, waste products and excess water are removed, while essential substances like sodium, potassium, and calcium are reabsorbed back into the bloodstream. This delicate balance helps to regulate blood pressure and maintain the body’s fluid and electrolyte levels.
In addition to their filtration duties, the kidneys also produce several important hormones. Erythropoietin, for example, stimulates the production of red blood cells in the bone marrow, ensuring that the body has an adequate supply of oxygen-carrying cells. The kidneys also activate vitamin D, which is crucial for maintaining strong, healthy bones and regulating the immune system’s response to infection.
RELATED: Patellar Tendonitis Explained: Diagnosis, Symptoms, and Treatment Options
Filtration process
The filtration process begins in the glomeruli, tiny clusters of blood vessels within each nephron. As blood enters the glomeruli, smaller molecules like waste products and excess fluid pass through the thin walls of the blood vessels and into the tubule. Larger molecules, such as proteins and blood cells, remain in the bloodstream.
The filtered fluid then flows through the tubule, where essential substances are reabsorbed back into the blood. This reabsorption process is carefully regulated by hormones and other signaling molecules, ensuring that the body retains the right amount of water, electrolytes, and nutrients. The remaining fluid and waste products become urine, which is stored in the bladder until it is expelled from the body.
Hormone production
In addition to erythropoietin and vitamin D, the kidneys produce several other hormones that have an impact on various bodily functions. Renin, an enzyme produced by the kidneys, plays a crucial role in regulating blood pressure through the renin-angiotensin system. When blood pressure drops, the kidneys release renin, which triggers a cascade of events that ultimately leads to an increase in blood pressure.
The kidneys also produce prostaglandins, hormone-like substances derived from lipids. These compounds have a wide range of effects on the body, including regulating inflammation, blood clotting, and smooth muscle contraction. Prostaglandins produced by the kidneys help to maintain healthy kidney function by regulating blood flow and salt and water balance.
Understanding the complex functions of the kidneys is essential for recognizing the signs and symptoms of kidney failure. When the kidneys are not working properly, waste products and excess fluid can build up in the body, leading to a host of health problems. By familiarizing themselves with the role of the kidneys and the hormones they produce, individuals can take steps to maintain kidney health and seek prompt medical attention if they suspect that their kidneys may be failing.
Types of Kidney Failure
Kidney failure can be classified into two main categories: acute kidney injury (AKI) and chronic kidney disease (CKD). The distinction between these two types is based on the onset and duration of the condition, as well as the underlying causes and potential for reversibility.
Acute kidney failure
Acute kidney injury, also known as acute kidney failure, is characterized by a sudden and rapid decline in kidney function. This type of kidney failure develops within a short period, usually over a few days or weeks. AKI is often triggered by a specific event or condition that leads to kidney malfunction, such as severe dehydration, blood loss from major surgery or injury, or the use of certain medications that are toxic to the kidneys.
The symptoms of acute kidney failure tend to appear suddenly and can be severe. These may include a rapid decrease in urine output, nausea, fatigue, swelling in the legs and feet, and shortness of breath. In some cases, AKI may not cause any noticeable symptoms and is only detected through blood tests while a person is hospitalized for another medical condition.
Treatment for acute kidney failure typically involves addressing the underlying cause and preventing complications. This may require hospitalization and interventions such as intravenous fluids to restore fluid balance, diuretics to reduce excess fluid, and hemodialysis to filter toxins from the blood. In most cases, acute kidney failure can be reversed once the underlying condition is treated, although some injuries may cause permanent damage leading to chronic kidney disease.
RELATED: Polycythemia Vera: From Diagnosis to Treatment – A Complete Guide
Chronic kidney failure
Chronic kidney disease, on the other hand, is a gradual and progressive loss of kidney function over an extended period, usually months or years. CKD is most commonly caused by long-term conditions that slowly damage the kidneys, such as diabetes, high blood pressure, and glomerulonephritis (inflammation of the kidney’s filtering units).
Unlike acute kidney failure, the symptoms of chronic kidney disease may not appear until the condition has advanced significantly. As kidney function declines, individuals may experience persistent fatigue, poor appetite, dry and itchy skin, swollen feet and ankles, frequent urination (especially at night), and difficulty concentrating. However, these symptoms can be easily mistaken for other conditions, making early detection challenging.
Treatment for chronic kidney disease focuses on managing the underlying cause and slowing the progression of kidney damage. This may involve medications to control high blood pressure and diabetes, dietary changes to reduce protein intake, and supplements to address complications such as anemia and bone disease. While chronic kidney disease is generally not reversible, proper management can help preserve remaining kidney function and delay the need for dialysis or a kidney transplant.
Causes and risk factors
Several factors can increase the risk of developing both acute and chronic kidney failure. Some of these risk factors are non-modifiable, such as a family history of kidney disease, older age, and certain genetic conditions like polycystic kidney disease. Other risk factors are related to underlying medical conditions, such as diabetes, heart disease, and obesity, which can contribute to kidney damage over time.
Additionally, lifestyle factors like smoking and long-term use of certain medications, including over-the-counter pain relievers, can also increase the risk of kidney failure. Recognizing these risk factors and taking steps to manage them, such as maintaining good blood sugar control in diabetes and reducing blood pressure, can help prevent or slow the progression of kidney disease.
Understanding the differences between acute and chronic kidney failure, as well as the underlying causes and risk factors, is crucial for early detection and appropriate management of these conditions. Regular check-ups with a healthcare provider and routine blood work can help identify kidney problems in their early stages, when treatment is most effective in preserving kidney function and preventing complications.
Recognizing Symptoms of Kidney Failure
Kidney failure, also known as end-stage renal disease (ESRD), can develop gradually over time, often without noticeable symptoms in the early stages. As the condition progresses, however, various signs and symptoms may emerge, indicating a decline in kidney function. Being aware of these symptoms is crucial for early detection and timely intervention to slow the progression of the disease and prevent complications.
Early warning signs
In the initial stages of kidney failure, symptoms may be subtle or nonspecific, making them easy to overlook or attribute to other conditions. Some of the early warning signs include:
- Changes in urination: Individuals may experience an increase or decrease in the amount of urine they produce, as well as changes in the appearance of their urine, such as foamy or dark-colored urine.
- Fatigue and weakness: As kidney function declines, the body may not be able to effectively remove waste products and toxins from the blood, leading to a general feeling of tiredness and lack of energy.
- Swelling in the legs, ankles, or feet: When the kidneys are not functioning properly, excess fluid can accumulate in the body, causing swelling (edema) in the lower extremities.
- Dry and itchy skin: Kidney failure can disrupt the balance of minerals in the body, leading to dry, itchy skin and other skin-related issues.
Advanced symptoms
As kidney failure progresses, more pronounced symptoms may develop, signaling a significant decline in kidney function. These advanced symptoms can have an impact on various aspects of an individual’s health and well-being, and may include:
- Nausea and vomiting: The buildup of waste products in the blood can cause feelings of nausea and lead to vomiting.
- Loss of appetite: As toxins accumulate in the body, individuals may experience a decrease in appetite and unintentional weight loss.
- Shortness of breath: Fluid buildup in the lungs, a condition known as pulmonary edema, can cause difficulty breathing and shortness of breath.
- Confusion and difficulty concentrating: High levels of toxins in the blood can affect cognitive function, leading to confusion, difficulty concentrating, and memory problems.
- Muscle cramps and twitches: Imbalances in electrolytes, such as potassium and calcium, can cause muscle cramps and involuntary twitches.
Complications
If left untreated, kidney failure can lead to a range of serious complications that can have a significant impact on an individual’s overall health and quality of life. Some of these complications include:
- Anemia: As kidney function declines, the body may not produce enough erythropoietin, a hormone that stimulates red blood cell production, leading to anemia and associated symptoms such as fatigue and weakness.
- Bone disease: Kidney failure can disrupt the balance of calcium and phosphorus in the body, leading to weakening of the bones and an increased risk of fractures.
- Heart disease: Individuals with kidney failure are at a higher risk of developing heart disease, as the buildup of waste products and fluid in the body can put additional strain on the cardiovascular system.
- Increased risk of infections: As kidney function declines, the body’s immune system may become compromised, making individuals more susceptible to infections.
Recognizing the symptoms of kidney failure is essential for early detection and timely intervention. If you experience any of these symptoms, especially if you have risk factors such as diabetes, high blood pressure, or a family history of kidney disease, it is important to consult with a healthcare provider for proper evaluation and management. Early diagnosis and treatment can help slow the progression of kidney failure and improve overall outcomes.
Diagnosis and Treatment Options
Diagnostic tests
Kidney failure is diagnosed through a combination of blood tests, urine tests, imaging tests, and kidney biopsy. Blood tests can measure the levels of waste products, such as creatinine and urea, in the blood, which increase when kidney function declines. Urine tests can detect abnormalities such as protein or blood in the urine, which may indicate kidney damage. Imaging tests, including ultrasound, CT scan, and MRI, can help identify structural abnormalities or blockages in the kidneys. In some cases, a kidney biopsy may be necessary to determine the cause of kidney failure and the extent of damage.
Medication and lifestyle changes
Treatment for kidney failure depends on the underlying cause and the severity of the condition. In the early stages of chronic kidney disease, treatment may focus on managing underlying conditions, such as diabetes and high blood pressure, through medication and lifestyle changes. Medications may be prescribed to control blood pressure, reduce cholesterol levels, treat anemia, and manage other complications of kidney disease. Lifestyle changes, such as adopting a low-sodium, low-protein diet, quitting smoking, and maintaining a healthy weight, can also slow the progression of kidney disease.
RELATED: Poison Hemlock: Detailed Guide on Identification and Control
Dialysis and transplantation
As kidney failure progresses, more aggressive treatment options may be necessary. Dialysis is a treatment that filters waste products and excess fluid from the blood when the kidneys can no longer perform this function. There are two main types of dialysis: hemodialysis and peritoneal dialysis. Hemodialysis involves using a machine to filter the blood outside the body, while peritoneal dialysis uses the lining of the abdomen to filter waste products from the blood inside the body. Kidney transplantation is another treatment option for end-stage kidney failure. It involves surgically placing a healthy kidney from a donor into the body to replace the damaged kidneys. A successful kidney transplant can eliminate the need for dialysis and improve quality of life. However, transplant recipients must take immunosuppressive medications for the rest of their lives to prevent rejection of the new kidney.
Conclusion
Understanding kidney failure and its implications has a profound impact on managing this complex health condition. This comprehensive guide has explored the essential functions of healthy kidneys, different types of kidney failure, common symptoms, and various treatment options. By shedding light on these aspects, individuals can better recognize early warning signs and seek timely medical attention to slow the progression of kidney disease.
To wrap up, kidney failure is a serious condition that requires careful management and ongoing medical care. With proper diagnosis, treatment, and lifestyle modifications, many people with kidney failure can maintain a good quality of life. Staying informed about kidney health and working closely with healthcare providers are crucial steps to address this challenging health issue effectively.