Ovarian cysts are a common health concern affecting many women worldwide. These fluid-filled sacs that develop on or inside the ovaries can cause discomfort and, in some cases, lead to more serious complications. Understanding the nature of ovarian cysts, their symptoms, and available treatments is crucial for women’s reproductive health and overall well-being.
This article aims to shed light on the various aspects of ovarian cysts. It will explore what ovarian cysts are, the common symptoms associated with them, and the underlying causes and risk factors. Additionally, it will discuss the diagnosis process and outline treatment options available to manage this condition. By providing this information, the article seeks to empower women with knowledge to better understand and address ovarian cysts.
What Are Ovarian Cysts?
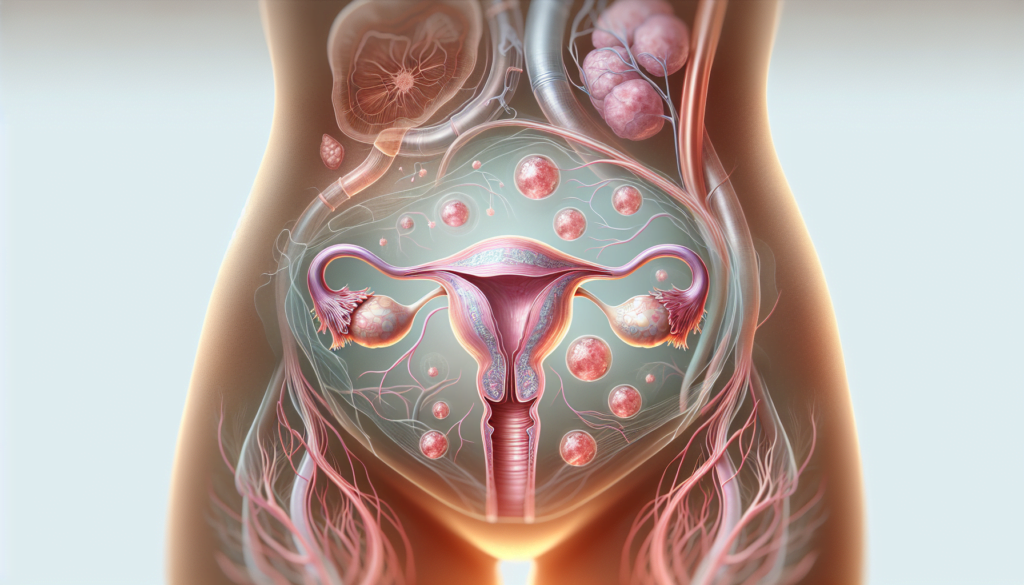
Ovarian cysts are fluid-filled sacs or pockets that form within or on the surface of one of the ovaries. Many women develop them at some point during their lives, and they are usually discovered during routine pelvic examinations. Most ovarian cysts are painless, cause no symptoms, and disappear on their own without the need for medical attention.
Definition
An ovarian cyst is a sac filled with fluid or semisolid material that forms on or within one or both of the ovaries. The ovaries are small organs in the pelvis that hold egg cells and make hormones, such as estrogen and progesterone.
RELATED: What is Arthus Reaction? Symptoms, Causes, and Treatment Options
Types of Ovarian Cysts
There are different types of ovarian cysts, most of which are painless and harmless (benign). The most common types include:
- Follicular cysts: A small sac in the ovary, called a follicle, releases an egg each month as part of the menstrual cycle. A follicular cyst forms when the follicle doesn’t release an egg and instead fills with fluid and grows bigger.
- Corpus luteum cysts: After the follicle releases an egg, it forms a hormone-producing group of cells called the corpus luteum. A cyst forms when fluid collects in the corpus luteum, causing it to grow.
- Cystadenomas: These cysts form on the surface of the ovary and can be filled with a watery liquid or a mucous material.
- Dermoid cysts (teratomas): These cysts contain tissue, such as hair, skin, fatty tissue, or teeth, and can grow quite large.
- Endometriomas: These cysts develop as a result of endometriosis, a condition in which uterine endometrial tissue grows outside the womb, causing cysts on the ovaries.
Functional vs. Pathological Cysts
Ovarian cysts can be categorized as either functional or pathological:
- Functional cysts: These are the most common type of ovarian cyst and aren’t disease-related. They occur as a result of ovulation (the release of an egg from the ovary) and are usually harmless, rarely cause pain, and often disappear on their own within two or three menstrual cycles.
- Pathological cysts: These cysts are less common and have formed as a result of abnormal cell growth rather than the normal function of the menstrual cycle. They can develop before and after menopause. While most pathological cysts are non-cancerous, a small number can be cancerous (malignant) and may require surgical removal.
Understanding the different types of ovarian cysts and their characteristics can help women better manage their reproductive health and seek appropriate medical care when necessary.
Common Symptoms of Ovarian Cysts
Many women with ovarian cysts do not experience any symptoms. However, when symptoms do occur, they can vary depending on the size and type of cyst. Some common symptoms associated with ovarian cysts include:
Pelvic Pain
One of the most common symptoms of ovarian cysts is pelvic pain. This pain can range from a dull ache to a sharp, sudden pain in the lower abdomen on the side of the cyst. The pain may come and go or be constant. In some cases, the pain can extend to the lower back and thighs.
Bloating
Ovarian cysts can cause a feeling of bloating or fullness in the abdomen. This symptom is more likely to occur with larger cysts that are taking up more space in the pelvic area. Some women may also experience swelling in the lower abdomen.
Menstrual Irregularities
Ovarian cysts can affect the menstrual cycle, leading to irregularities such as heavy or irregular periods. Some women may experience lighter periods than normal or miss their periods altogether. Pain during menstruation can also be a symptom of ovarian cysts.
RELATED: Understanding Arthrogryposis: Causes, Symptoms, and Treatments
Other Symptoms
In addition to the above symptoms, ovarian cysts may cause other less common symptoms, such as:
- Nausea and vomiting
- Pain during sexual intercourse
- Frequent urination or difficulty emptying the bladder
- Unexplained weight gain
- Breast tenderness
It is important to note that these symptoms can also be caused by other conditions, so it is essential to consult with a healthcare provider for an accurate diagnosis. In rare cases, ovarian cysts can rupture or cause the ovary to twist (ovarian torsion), leading to severe pain and requiring immediate medical attention.
Causes and Risk Factors
Several factors can contribute to the development of ovarian cysts, including hormonal imbalances, endometriosis, pregnancy, and pelvic infections. Understanding these causes and risk factors is crucial for identifying and managing ovarian cysts effectively.
Hormonal Imbalances
Hormonal imbalances play a significant role in the formation of ovarian cysts. Infertility treatments that involve the use of other ovulation induction agents may lead to the development of cysts as part of ovarian hyperstimulation syndrome. Additionally, medications and conditions such as hypothyroidism can also contribute to cyst formation.
Endometriosis
Endometriosis is a chronic condition where endometrial tissue grows outside the uterus, often on the ovaries. When endometrial tissue grows inside the ovaries, it can form cavities filled with blood, known as endometriomas or “chocolate cysts.” These cysts are associated with pain before, during, and after menstruation, which is a common symptom of endometriosis.
Pregnancy
Ovarian cysts can develop during pregnancy, particularly in the second trimester when human chorionic (hCG) levels peak. The most common type of ovarian cyst during pregnancy is a corpus luteum cyst. Rather than shrinking, the follicle that released the egg fills with fluid and remains on the ovary. These cysts usually resolve on their own by the middle of the second trimester.
Pelvic Infections
Pelvic infections, such as pelvic inflammatory disease (PID), can contribute to the development of ovarian cysts. Bacteria from the infection can spread from the cervix to the ovaries, causing cysts to form. These cysts are filled with bacteria and can lead to serious complications, such as sepsis, if they rupture.
Other risk factors for ovarian cysts include:
- Early menarche (before 11-13 years old)
- Late menopause and short menstrual cycles (less than 27 days)
- Cigarette smoking
- Tubal ligation sterilization
Being aware of these causes and risk factors can help women and their healthcare providers identify and manage ovarian cysts more effectively, reducing the risk of complications and promoting overall reproductive health.
Diagnosis and Treatment Options
Diagnosing ovarian cysts involves a combination of physical examination and imaging tests. The treatment approach depends on factors such as the size of the cyst, the presence of symptoms, and the risk of malignancy.
Physical examination includes a pelvic exam to determine the location, shape, size, and mobility of the cyst. However, the ability to diagnose ovarian cysts through pelvic examination is limited, as it depends on the patient’s body habitus, provider experience, and pelvic anatomy.
Imaging tests play a crucial role in the evaluation of ovarian cysts. Transvaginal ultrasonography is the most common and preferred imaging modality for initial assessment. It helps differentiate between benign and malignant masses by evaluating characteristics such as laterality, size, composition (cystic, solid, or mixed), presence of septations, papillary excrescences, mural nodules, pelvic free fluid, and vascularity via color doppler.
Findings suggestive of benign cysts include thin, smooth walls, absence of septations, solid components, and internal flow on color doppler. On the other hand, cyst size greater than 10 cm, complex multilocular mass, papillary excrescences or solid components, irregularity, thick septations, ascites, and increased vascularity raise suspicion for malignancy and warrant further evaluation.
RELATED:Arthritis of the Knee: Comprehensive Guide to Symptoms and Treatments
Additional imaging studies like magnetic resonance imaging (MRI) or computed tomography (CT) can be performed but are not recommended as part of the initial evaluation. Gynecologic oncology consultation should be considered in cases suspicious for malignancy.
Treatment options for ovarian cysts include:
- Watchful waiting: For asymptomatic cysts that are initially classified as benign by ultrasound, a period of close observation without intervention is often recommended. This involves regular ultrasounds and self-monitoring. If the cyst does not resolve after several menstrual cycles, further workup is indicated.
- Medications: Oral contraceptive pills (OCPs) protect against the development of functional ovarian cysts but cannot be used to resolve existing ones. Pain management with nonsteroidal anti-inflammatory drugs (NSAIDs) or narcotic analgesics may be necessary for symptomatic relief.
- Surgical interventions: Large or persistent ovarian cysts, symptomatic cysts, or those with concerning features for malignancy usually require surgical removal. Laparoscopic ovarian cystectomy is the preferred approach for most cases, as it is minimally invasive and associated with faster recovery. Open cystectomy (laparotomy) may be necessary for large cysts or when malignancy is suspected.
The choice of treatment depends on individual factors such as the patient’s age, menopausal status, cyst size, presence of symptoms, and risk of malignancy. A multidisciplinary approach involving gynecologists, radiologists, and gynecologic oncologists is essential for optimal management of ovarian cysts.
Conclusion
Ovarian cysts are a common health issue that has an impact on many women’s lives. This article has explored the different types of cysts, their symptoms, causes, and available treatments to provide a comprehensive understanding of this condition. By shedding light on the various aspects of ovarian cysts, from hormonal imbalances to diagnostic methods, we’ve aimed to equip women with the knowledge to address this health concern effectively.
While most ovarian cysts are harmless and resolve on their own, being aware of the signs and risk factors is crucial to maintaining good reproductive health. Regular check-ups and open communication with healthcare providers are key to managing ovarian cysts and ensuring overall well-being. With the right information and medical care, women can navigate this common health issue with confidence and peace of mind.