Perianal infection is a painful and uncomfortable condition that affects the area around the anus. This common problem can have a significant impact on a person’s quality of life, causing discomfort and potentially leading to more serious complications if left untreated. Perianal abscesses, a type of infection that forms pockets of pus near the anus, are particularly troublesome and require prompt medical attention.
Understanding the symptoms, causes, and treatment options for perianal infections is crucial to manage this condition effectively. This article aims to shed light on the pathophysiology of perianal abscesses, explore the clinical presentation of these infections, and discuss various treatment approaches. By delving into these aspects, readers will gain valuable insights to recognize and address perianal infections promptly, potentially avoiding more severe health issues down the line.
Pathophysiology of Perianal Abscesses
Formation of abscesses
The development of perianal abscesses typically begins with an infection in the anal crypts and glands located at the base of the anal canal. These glands, which secrete mucus to lubricate the anal canal, can become clogged with debris, leading to bacterial overgrowth and subsequent infection. As the infection progresses, pus and fluid accumulate within the anal gland, causing it to swell and form a painful abscess. The internal anal sphincter muscle usually acts as a barrier, preventing the spread of infection from the anal lumen to the deeper perirectal tissues. However, the infection can breach this barrier through the crypts of Morgagni, which are small ducts that can penetrate the internal sphincter and provide a pathway for the infection to reach the intersphincteric space.
Bacterial involvement
Perianal abscesses are often polymicrobial, involving a diverse range of bacterial species. Metagenomic next-generation sequencing (mNGS) studies have revealed a complex microbial landscape in these abscesses, with an average of 6.1 different bacterial taxa per abscess sample. The most commonly identified bacteria include Bilophila wadsworthia (71.4%), Bacteroides fragilis (57.1%), and Escherichia coli (50.0%). Other frequently detected species are Bacteroides thetaiotaomicron, Prevotella bivia, Prevotella timonensis, and Streptococcus constellatus, each found in 28.6% of perianal abscess patients. Gram-negative anaerobic bacteria appear to be the predominant pathogens in perianal infections. Interestingly, although Bilophila wadsworthia is the most frequently detected species, it is usually present in lower abundance compared to Bacteroides fragilis and Escherichia coli, which exhibit significantly higher abundance in the abscess samples.
RELATED: Managing Dermatographia: Tips and Treatments for Relief
Spread of infection
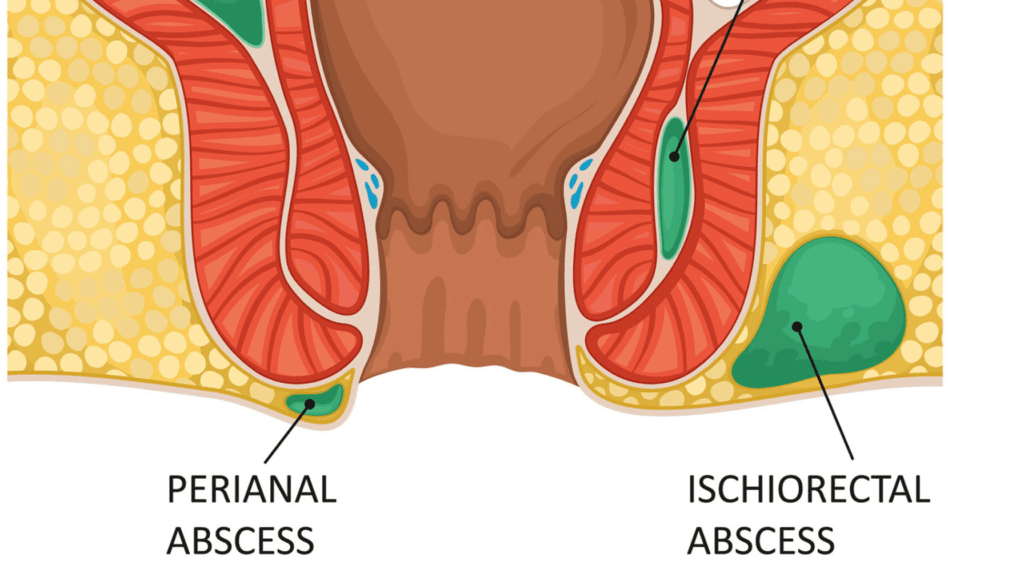
Once the infection gains access to the intersphincteric space, it can easily spread to the adjacent perirectal spaces, leading to the formation of abscesses in various locations. The infection may extend into the intersphincteric space, ischiorectal space, or even the supralevator space. In some cases, the abscess remains contained within the intersphincteric space. The severity and depth of the abscess can vary considerably, and the abscess cavity is often associated with the formation of a fistulous tract. A fistula is an abnormal tunnel that connects the infected anal gland to the skin surface near the anus. If left untreated, perianal abscesses can lead to the development of anal fistulas, which may require additional surgical intervention. Prompt diagnosis and treatment of perianal abscesses are crucial to prevent the spread of infection and minimize the risk of complications such as fistula formation or systemic infection.
Clinical Presentation
The clinical presentation of a perianal abscess can vary depending on the location and severity of the infection. Patients typically experience a range of symptoms that can significantly impact their quality of life. Recognizing these signs and symptoms is crucial for prompt diagnosis and treatment, as untreated perianal infections can lead to serious complications.
Typical symptoms
The most common symptom of a perianal abscess is severe, throbbing pain in the anal area. This pain often intensifies when sitting, during bowel movements, or with physical activity. Patients may also experience swelling, redness, and tenderness in the affected area. In some cases, the abscess may cause fever, chills, and a general feeling of malaise. These systemic symptoms are more likely to occur with deeper abscesses, such as those in the intersphincteric or supralevator spaces.
Other symptoms may include constipation or painful bowel movements, as the inflammation and swelling can make defecation difficult and uncomfortable. Some patients may notice drainage of pus or blood from the perianal area, particularly if the abscess has ruptured spontaneously. Rectal bleeding, although less common, can also occur due to the pressure and inflammation caused by the abscess.
Physical examination findings
During a physical examination, healthcare providers will visually inspect the perianal area for signs of infection. They may observe a swollen, red, and tender mass near the anal opening. In some cases, the abscess may have already drained, leaving behind a small opening or ulceration in the skin.
A digital rectal examination is an essential part of the diagnostic process. The healthcare provider will gently insert a gloved, lubricated finger into the rectum to assess for any abnormalities. They may palpate a firm, tender mass or an area of fluctuance, indicating the presence of pus. However, it is important to note that deeper abscesses, such as those in the intersphincteric or supralevator spaces, may not be palpable on digital rectal examination.
In some cases, the healthcare provider may need to perform an examination under anesthesia to thoroughly evaluate the extent of the infection and to determine the most appropriate treatment approach. This is particularly important for patients with severe pain or those suspected of having deep or complex abscesses.
RELATED: Delirium Tremens: In-depth Guide to Symptoms, Risks, and Care
Differential diagnosis
When evaluating a patient with symptoms suggestive of a perianal abscess, healthcare providers must consider several other conditions that can present similarly. These include:
- Anal fissure: A tear in the lining of the anal canal that can cause severe pain, especially during bowel movements.
- Thrombosed external hemorrhoid: A blood clot that forms within an external hemorrhoid, causing acute pain and swelling.
- Pilonidal cyst: An infected cyst or abscess that develops in the crease of the buttocks, often due to ingrown hairs.
- Hidradenitis suppurativa: A chronic inflammatory skin condition that can cause painful, recurrent abscesses in the groin and perianal areas.
- Sexually transmitted infections: Certain STIs, such as herpes simplex virus or syphilis, can cause ulcerations or lesions in the perianal region.
- Anal or rectal cancer: Although rare, malignancies in the anal or rectal area can present with symptoms similar to those of a perianal abscess.
Accurately diagnosing a perianal abscess is crucial for initiating appropriate treatment and preventing complications. Healthcare providers will rely on a combination of the patient’s history, physical examination findings, and, in some cases, imaging studies to differentiate between a perianal abscess and other conditions. By promptly recognizing the signs and symptoms of this painful condition, healthcare professionals can ensure that patients receive the care they need to achieve a full recovery and maintain their quality of life.
Treatment Options
Incision and drainage
The primary treatment for perianal abscesses is prompt incision and drainage. This procedure is typically performed in an outpatient setting under local anesthesia. The goal is to create an opening in the abscess to allow the pus and infected material to drain, relieving pressure and promoting healing. The incision is usually made as close as possible to the anal verge to minimize the potential for developing a chronic fistula. In some cases, a cruciate (cross-shaped) incision may be used to ensure adequate drainage. After the abscess is drained, the cavity is thoroughly cleaned and irrigated with saline solution. Packing the wound with gauze is sometimes done to prevent premature closure and promote continued drainage, although the necessity of this practice is debated.
For larger or deeper abscesses, such as those in the intersphincteric or supralevator spaces, surgical drainage under general anesthesia may be necessary. In these cases, the surgeon will perform an examination under anesthesia to assess the extent of the abscess and determine the best approach for drainage. A catheter may be placed in the abscess cavity to facilitate ongoing drainage, especially in patients with severe systemic illness, diabetes, or morbid obesity.
Antibiotic therapy
The role of antibiotics in the treatment of perianal abscesses is limited. In most cases, drainage of the abscess is sufficient to control the infection without the need for systemic antibiotics. However, antibiotic therapy may be considered in certain situations, such as:
- Patients with significant cellulitis surrounding the abscess
- Immunocompromised individuals
- Patients with underlying medical conditions that increase the risk of complications, such as diabetes or inflammatory bowel disease
- Cases where the infection has spread beyond the initial abscess site
When antibiotics are prescribed, they should provide broad-spectrum coverage against the common causative organisms, including gram-negative anaerobes, Escherichia coli, and Staphylococcus aureus. A combination of amoxicillin-clavulanate or ciprofloxacin plus metronidazole for 7-10 days is often recommended. Obtaining wound cultures can help guide antibiotic selection, particularly in patients who have previously received antibiotics or have known drug resistance.
It is important to note that antibiotics alone are not an adequate substitute for surgical drainage of perianal abscesses. Prompt incision and drainage remain the cornerstone of treatment, with antibiotics serving as an adjunctive therapy in select cases.
RELATED: DiGeorge Syndrome Overview: Symptoms, Causes, and Treatments
Postoperative care
After the incision and drainage procedure, proper postoperative care is essential to promote healing and prevent complications. Patients should be advised to:
- Take warm sitz baths several times a day to soothe the area and promote drainage
- Keep the perianal region clean and dry, gently cleansing the area after each bowel movement
- Use stool softeners or fiber supplements to prevent constipation and minimize straining during bowel movements
- Take prescribed pain medications as needed to manage discomfort
- Attend follow-up appointments with their healthcare provider to monitor healing progress
Patients should be informed that complete healing may take several weeks and that some degree of drainage is expected during this time. They should also be educated about the potential for developing a chronic fistula and instructed to report any persistent drainage, pain, or other concerning symptoms to their healthcare provider.
In cases where a perianal fistula is identified during the initial treatment of the abscess, additional interventions may be necessary. These may include fistulotomy (surgical opening of the fistula tract), seton placement (a surgical thread left in place to promote drainage), or more complex surgical procedures depending on the location and complexity of the fistula. The management of perianal fistulas often requires a multidisciplinary approach involving colorectal surgeons, gastroenterologists, and wound care specialists to optimize outcomes and minimize the risk of recurrence.
Conclusion
To wrap up, perianal infections, particularly abscesses, are painful conditions that have a significant impact on a patient’s quality of life. Early diagnosis and proper treatment are crucial to prevent complications and promote healing. The cornerstone of treatment is incision and drainage, which relieves pain and allows the infection to clear. In some cases, antibiotics may be necessary, especially for patients with certain risk factors or extensive infections.
Proper post-operative care plays a key role in recovery and helps to prevent recurrence. Patients should be aware of the potential for fistula development and report any persistent symptoms to their healthcare provider. By understanding the causes, symptoms, and treatment options for perianal infections, individuals can seek timely medical attention and improve their chances of a full recovery. This knowledge empowers patients to take an active role in their health and well-being.