Placenta previa is a serious pregnancy complication that affects expectant mothers and their unborn babies. This condition occurs when the placenta partially or completely covers the cervix, potentially causing severe bleeding during pregnancy or childbirth. Understanding placenta previa is crucial for pregnant women and healthcare providers to ensure proper management and reduce the risks associated with this condition.
This article delves into the various aspects of placenta previa, including its symptoms, causes, and available treatments. It explores the warning signs that pregnant women should watch out for, the diagnostic procedures used to identify the condition, and the management strategies employed by medical professionals. By shedding light on this important topic, readers will gain valuable insights to help them navigate this challenging pregnancy complication.
Understanding Placenta Previa
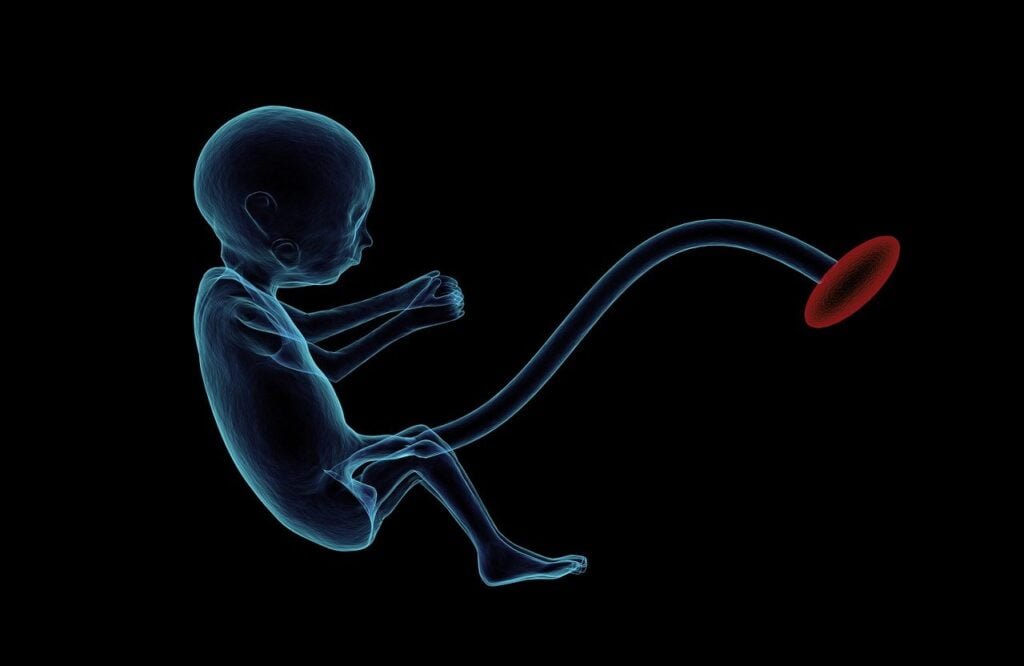
Placenta previa is a serious pregnancy complication that occurs when the placenta partially or completely covers the cervix, potentially causing severe bleeding during pregnancy or childbirth. The placenta is a temporary organ that develops in the uterus during pregnancy, providing oxygen and nutrients to the growing fetus through the umbilical cord.
Anatomy of the Placenta
The placenta is a disc-shaped organ that attaches to the uterine wall and connects to the fetus via the umbilical cord. It is composed primarily of blood vessels that allow for the exchange of oxygen, nutrients, and waste products between the mother’s and baby’s bloodstreams. The placenta also produces hormones essential for fetal growth and development.
RELATED: How to Identify and Remove Tonsil Stones: A Complete Guide
How Placenta Previa Develops
In most pregnancies, the placenta implants at the top or side of the uterus. However, in placenta previa, it implants lower in the uterus, near or covering the cervical opening. The exact cause of placenta previa is unknown, but it is associated with certain risk factors such as previous cesarean deliveries, advanced maternal age, smoking, and a history of placenta previa in prior pregnancies.
Prevalence and Statistics
Placenta previa affects approximately 0.3% to 2% of pregnancies in the third trimester. The prevalence has increased in recent years, likely due to the rising rates of cesarean sections. Women with a history of cesarean deliveries have a higher risk of developing placenta previa in subsequent pregnancies.
The presence of placenta previa can lead to complications such as preterm birth, low birth weight, and the need for cesarean delivery. In some cases, placenta previa may be associated with placenta accreta spectrum (PAS) disorders, where the placenta abnormally attaches to or invades the uterine wall, further increasing the risk of severe bleeding and other complications.
Recognizing the Signs
The main sign of placenta previa is bright red vaginal bleeding, usually without pain, after 20 weeks of pregnancy. Sometimes, spotting happens before an event with more blood loss. The bleeding may occur with prelabor contractions of the uterus that cause pain. The bleeding may also be triggered by sex or during a medical exam. For some women, bleeding may not occur until labor. Often there is no clear event that leads to bleeding.
Early Warning Signs
In the early stages of placenta previa, pregnant women may experience light, painless vaginal bleeding. This bleeding can be intermittent, starting and stopping over a period of days or weeks. It is crucial to report any vaginal bleeding during pregnancy to a healthcare provider, as it can be a sign of placenta previa or other complications.
Emergency Symptoms
As placenta previa progresses, the bleeding can become more severe and potentially life-threatening. Emergency symptoms include:
- Heavy, bright red vaginal bleeding
- Persistent uterine contractions
- Abdominal pain or tenderness
- Dizziness or fainting due to blood loss
If any of these symptoms occur, it is essential to seek immediate medical attention.
Differentiating from Other Conditions
Placenta previa can be mistaken for other pregnancy complications that cause vaginal bleeding, such as:
- Placental abruption: A condition where the placenta partially or completely separates from the uterine wall before delivery.
- Preterm labor: Labor that begins before 37 weeks of pregnancy.
- Miscarriage: The loss of a pregnancy before 20 weeks gestation.
To differentiate placenta previa from these conditions, healthcare providers will perform a thorough evaluation, including a physical exam, ultrasound, and possibly other diagnostic tests. Accurately identifying placenta previa is crucial for proper management and treatment to ensure the best possible outcomes for both mother and baby.
Diagnostic Procedures
The diagnosis of placenta previa involves a combination of ultrasound techniques and careful clinical evaluation. Routine sonography in the first and second trimester of pregnancy provides early identification of this condition. While the initial diagnosis may be made with a transabdominal ultrasound, a transvaginal ultrasound is considered the gold standard for confirming the location of the placenta.
Ultrasound Techniques
Transvaginal ultrasound is superior to transabdominal ultrasound in accurately diagnosing placenta previa. It provides clear images of the placenta’s position relative to the cervix, with false-positive and false-negative rates of 1.0% and 2.0%, respectively. The procedure is safe and well-tolerated by patients. Transabdominal ultrasound, although less accurate, can be used in conjunction with transvaginal ultrasound or as an alternative when necessary.
RELATED: Scabies: Comprehensive Guide to Symptoms and Treatments
Other Imaging Methods
In cases of posterior placenta previa or when there is a need to assess potential invasion to the bladder, magnetic resonance imaging (MRI) may be utilized. However, MRI is costly and has not been shown to improve diagnosis or outcomes compared to ultrasonography alone.
Avoiding Invasive Examinations
When placenta previa is suspected, it is crucial to avoid digital examinations or any manipulation of the placenta, as this can lead to severe hemorrhage. A thorough abdominal examination to identify uterine tenderness can help differentiate other causes of vaginal bleeding, such as uterine rupture or placental abruption.
In addition to imaging, laboratory tests such as Rh compatibility, fibrin split products, fibrinogen levels, prothrombin time, activated partial thromboplastin time, blood type and cross-match, and complete blood count are indicated in women with suspected placenta previa. These tests help assess the mother’s blood clotting ability and prepare for potential blood transfusions if needed.
Managing Placenta Previa
The management of placenta previa focuses on minimizing the risk of bleeding and ensuring the safety of both the mother and the baby. Treatment approaches vary depending on the severity of the condition and the stage of pregnancy.
Hospital Care
Women with placenta previa who experience vaginal bleeding may require hospitalization for close monitoring and treatment. During the hospital stay, the healthcare team will:
- Monitor the mother’s vital signs and the baby’s well-being
- Administer intravenous fluids and blood transfusions, if necessary
- Prescribe medications to prevent premature labor and promote fetal lung maturity
- Perform regular ultrasounds to assess the placenta’s position and the baby’s growth
In cases of severe bleeding or if the pregnancy has reached 36 weeks, an emergency cesarean delivery may be necessary.
Home Care Instructions
For women with placenta previa who are not actively bleeding, home care instructions may include:
- Avoiding sexual intercourse and any activities that may trigger contractions or bleeding
- Limiting physical activity and avoiding heavy lifting
- Staying near a hospital with a neonatal intensive care unit (NICU)
- Attending regular prenatal check-ups and monitoring appointments
- Reporting any signs of bleeding, contractions, or decreased fetal movement to the healthcare provider immediately
Adherence to these home care instructions can help reduce the risk of complications and prolong the pregnancy until a safe delivery can be performed.
RELATED: Syphilis: Key Symptoms, Diagnosis Methods, and Treatment
Preparing for Delivery
As the pregnancy progresses, the healthcare team will develop a delivery plan based on the placenta’s position and the mother’s condition. In most cases, a scheduled cesarean section will be necessary to avoid the risks associated with vaginal delivery.
The timing of the cesarean section depends on several factors:
- Severity of placenta previa
- Presence of bleeding episodes
- Fetal growth and well-being
- Maternal health conditions
Typically, a cesarean section is planned between 36 and 37 weeks of gestation to minimize the risk of spontaneous labor and bleeding. In some cases, corticosteroids may be administered to accelerate fetal lung maturity before delivery.
By closely managing placenta previa through hospital care, home care instructions, and a well-planned delivery, healthcare providers aim to optimize outcomes for both the mother and the baby.
Conclusion
Placenta previa has a significant impact on pregnancy, posing risks to both mother and baby. Understanding its symptoms, causes, and management strategies is crucial to ensure the best possible outcomes. Early detection through routine ultrasounds and proper medical care can greatly reduce the complications associated with this condition. Healthcare providers play a key role in guiding expectant mothers through this challenging situation, offering tailored treatment plans and support.
For women diagnosed with placenta previa, close monitoring and adherence to medical advice are essential. While the condition can be stressful, advances in medical care have improved the outlook for affected pregnancies. By working closely with their healthcare team and following recommended precautions, many women with placenta previa can successfully navigate their pregnancy and deliver healthy babies. The journey may be challenging, but with proper care and support, positive outcomes are often achievable.