Varicocele is a common condition that affects many men, yet it often goes unnoticed or misunderstood. This medical issue involves the enlargement of veins within the scrotum, which can have an impact on male fertility and overall testicular health. While it may sound alarming, varicocele is typically treatable and manageable with proper medical care.
Understanding varicocele is crucial to recognize its symptoms, identify potential causes, and explore available treatment options. This article aims to shed light on the key aspects of varicocele, including its definition, common signs, risk factors, and diagnostic procedures. Additionally, it will discuss various treatment approaches to help men make informed decisions about their reproductive health and well-being.
What is a Varicocele?
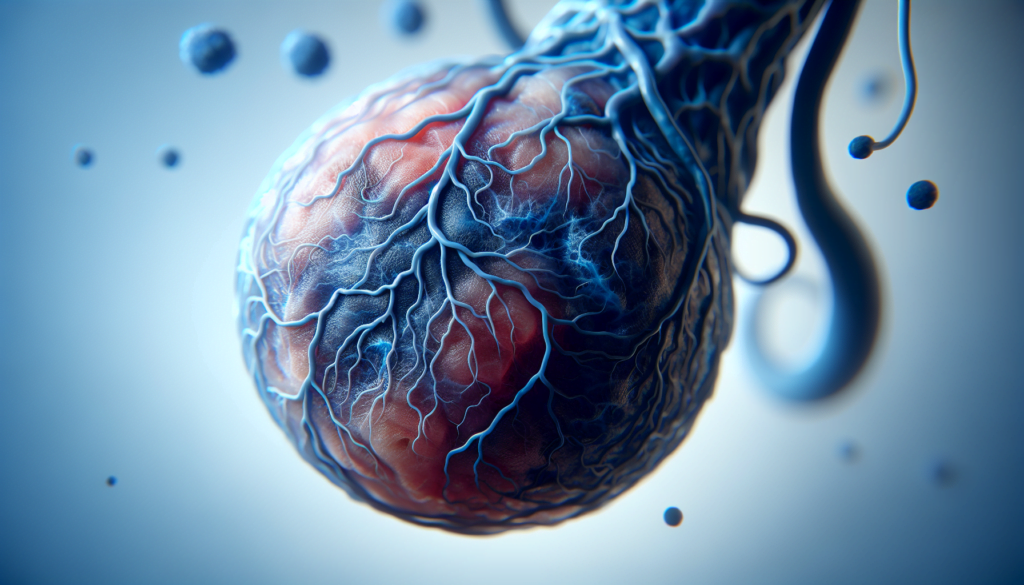
A varicocele is an abnormal enlargement of the veins within the scrotum, the loose bag of skin that holds the testicles. These dilated veins, known as the pampiniform plexus, are similar to varicose veins that can occur in the legs. Varicoceles are a common condition, particularly in young men between the ages of 15 and 25.
Definition
Varicoceles are defined as abnormally dilated veins that drain blood from the testicles. They occur when the valves within these veins fail to function properly, causing blood to pool and the veins to enlarge. This can lead to a range of symptoms and potential complications, including pain, testicular atrophy, and infertility.
RELATED: Athetoid Cerebral Palsy: Detailed Symptoms and Treatment Options
Anatomy
Varicoceles most commonly develop in the left testicle, likely due to the anatomical structure of the left testicular vein. The left testicular vein drains into the left renal vein at a right angle, which can increase the pressure within the vein and lead to valve failure. In contrast, the right testicular vein drains directly into the inferior vena cava, reducing the risk of varicocele formation on the right side.
Prevalence
Varicoceles are a prevalent condition, affecting approximately 15% of all men. The incidence of varicocele increases with age, with the condition being most common in men between the ages of 15 and 25. Varicoceles are also more frequently diagnosed in men with fertility issues, with an estimated 35% of men with primary infertility and up to 80% of men with secondary infertility having a varicocele.
Symptoms of Varicocele
Many men with varicocele may not experience any noticeable symptoms. However, when symptoms do occur, they can have an impact on physical comfort and fertility. The most common signs and symptoms associated with varicocele include:
Physical signs
A varicocele often presents as a visible or palpable mass in the scrotum. It may appear as a swelling or enlargement of the veins, resembling a “bag of worms.” The affected testicle may also shrink in size, a condition known as testicular atrophy. In some cases, the varicocele may only be detectable during a physical examination by a healthcare provider.
Pain and discomfort
Some men with varicocele may experience pain or discomfort in the scrotum, particularly when standing or engaging in physical activities for extended periods. The pain is often described as a dull ache or a feeling of heaviness in the testicles. Lying down or elevating the feet can help alleviate the discomfort, as it reduces the pressure on the affected veins.
Fertility issues
Varicocele has been identified as a common cause of male infertility. The presence of a varicocele can have an adverse effect on sperm quality, including decreased sperm count, reduced sperm motility, and an increase in the number of abnormal sperm. These factors can contribute to difficulty conceiving. Approximately 30% of infertile men have a varicocele, highlighting the significant role this condition plays in male reproductive health.
It is important to note that the severity of symptoms does not always correlate with the size of the varicocele. Even small varicoceles can have a significant impact on fertility. If you experience any of these symptoms or have concerns about your reproductive health, it is advisable to consult with a healthcare provider for a proper evaluation and discussion of treatment options.
Causes and Risk Factors
The exact causes of varicocele are not fully understood, but several factors contribute to its development. The primary cause is believed to be faulty valves in the veins that drain blood from the testicles. When these valves fail to function properly, blood can pool in the veins, causing them to enlarge and become varicoceles.
Blood flow issues play a significant role in the formation of varicoceles. The left testicular vein, which connects to the left renal vein at a right angle, is more prone to increased pressure. This anatomical structure makes the left testicle more susceptible to varicocele development compared to the right testicle.
RELATED: Atherosclerosis of Aorta: Diagnosis and Treatment Options
Genetic predisposition may also influence the occurrence of varicoceles. Studies have shown that varicoceles tend to run in families, suggesting a hereditary component. Men with a family history of varicocele, especially in first-degree relatives such as fathers or brothers, have an increased risk of developing the condition.
Other potential risk factors for varicocele include:
- Age: Varicoceles often develop during puberty, when the testicles experience rapid growth and require increased blood supply.
- Obesity: Excess body weight can put additional pressure on the veins in the scrotum, increasing the likelihood of varicocele formation.
- Occupations involving prolonged standing or heavy lifting: These activities can exert pressure on the veins and contribute to the development of varicoceles.
It is important to note that having one or more risk factors does not necessarily mean an individual will develop a varicocele. Conversely, some men may develop varicoceles without any identifiable risk factors. Regular self-examination and routine physical examinations by a healthcare provider can help detect varicoceles early, allowing for timely management and treatment.
Diagnosis and Treatment Options
The diagnosis of varicocele typically involves a physical examination and imaging tests. Treatment options include surgical procedures and non-surgical alternatives, depending on the severity and symptoms of the condition.
Physical examination is the standard diagnostic test for varicoceles. The examination is performed by inspecting and palpating the scrotum while the patient is standing. Varicoceles are graded based on their visibility and palpability, with Grade I being palpable only with Valsalva maneuver, Grade II being palpable without Valsalva, and Grade III being readily visible through the scrotal skin.
Imaging tests, such as scrotal ultrasound, can be helpful when the physical examination is difficult or indeterminate. Ultrasound criteria for varicocele include dilation of spermatic veins and demonstration of reversal of flow with color Doppler. However, the routine use of ultrasound for varicocele diagnosis is not recommended.
RELATED: Understanding Atherosclerosis: Symptoms, Causes, and Treatments
Treatment options for varicocele include surgical procedures and non-surgical alternatives. The most common surgical approaches are:
- Microsurgical subinguinal varicocelectomy: Considered the current surgical standard, this approach involves making a small incision below the external inguinal ring and using a microscope to identify and ligate the dilated veins while preserving the testicular artery and lymphatics.
- Laparoscopic varicocelectomy: This minimally invasive approach involves ligating the spermatic veins near the entry point into the left renal vein using a laparoscope.
- Open retroperitoneal (Palomo) and inguinal (Ivanissevich) approaches: These traditional open surgical techniques involve ligating the spermatic veins at higher levels, with the retroperitoneal approach being less commonly used due to higher recurrence and complication rates.
Non-surgical alternatives for varicocele treatment include percutaneous embolization and sclerotherapy. Embolization involves blocking the affected veins by creating a tiny dam using coils or a sclerosing solution, which redirects blood flow to healthy veins. This procedure is performed by an interventional radiologist and has been shown to be as effective as surgery with less risk, pain, and recovery time.
The choice of treatment depends on various factors, including the grade of varicocele, presence of symptoms, and the patient’s desire for future fertility. Consultation with a urologist, particularly one specializing in male infertility, can help determine the most appropriate course of action for each individual case.
Conclusion
Varicoceles have a significant impact on men’s reproductive health, affecting both physical comfort and fertility. This condition, characterized by enlarged veins in the scrotum, can lead to pain, testicular shrinkage, and reduced sperm quality. Understanding the symptoms, causes, and available treatments is crucial to manage this common issue effectively. Early detection through regular self-exams and professional check-ups can make a big difference in addressing varicoceles promptly.
For men dealing with varicoceles, there are several treatment options to consider. These range from surgical procedures like microsurgical varicocelectomy to non-surgical alternatives such as embolization. The choice of treatment depends on the severity of the condition, the presence of symptoms, and individual fertility goals. Consulting with a urologist, especially one who specializes in male infertility, is key to figure out the best approach for each case. With proper care and management, many men can overcome the challenges posed by varicoceles and improve their overall reproductive health.