Insulin resistance is a burgeoning health issue that silently paves the way for more complex conditions like type 2 diabetes and prediabetes, impacting millions globally. This condition, where the body’s cells do not respond effectively to insulin, can lead to a cascade of health challenges, yet many remain unaware of its significance. Understanding what insulin resistance is, its symptoms, and its long-term effects is pivotal for managing and potentially reversing its impact. Recognizing the early signs of insulin resistance could mean the difference between proactive health management and the onset of more severe diseases.
This article dives into the intricacies of insulin resistance, exploring its causes, the symptoms to be vigilant of, and the critical link between insulin resistance and type 2 diabetes. Furthermore, it will provide insight into the diagnosis of insulin resistance and the latest approaches in treatment and management, including lifestyle modifications like weight loss and dietary adjustments. By giving a comprehensive overview, from identifying early signs of insulin resistance to implementing effective solutions, this article aims to equip readers with the knowledge needed to address this silent health issue head-on.
What is Insulin Resistance?
Understanding Insulin Resistance
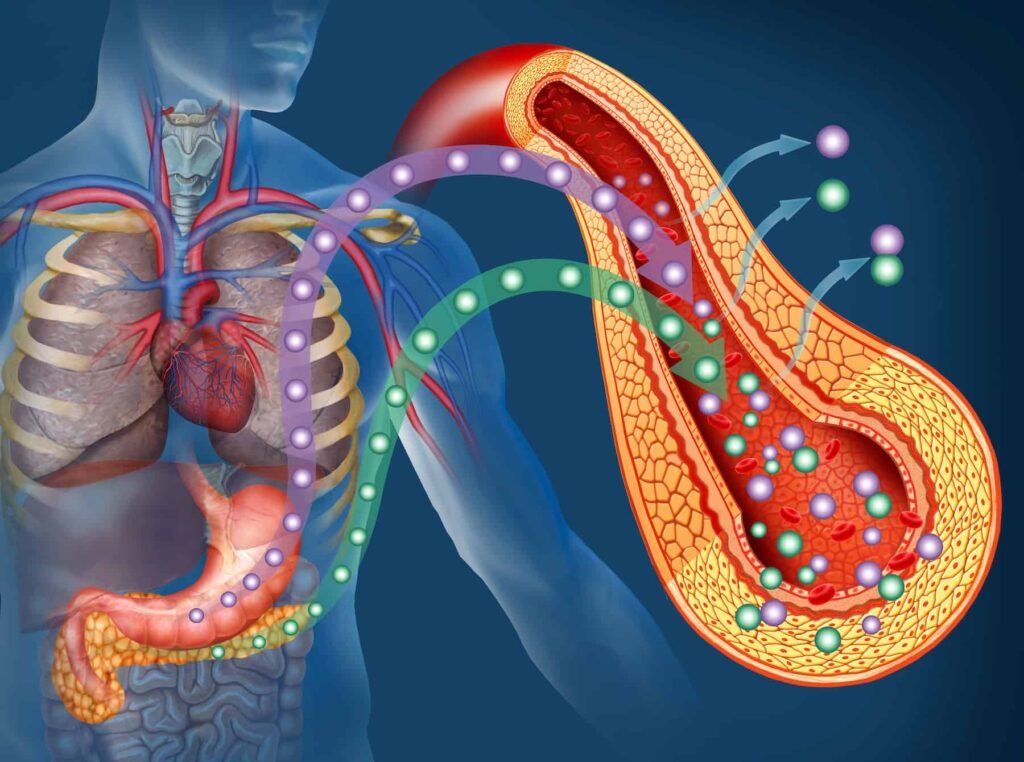
Insulin resistance is a condition where the body’s cells do not respond effectively to insulin, a hormone produced by the pancreas that is vital for regulating blood glucose levels. This resistance can occur in muscle, fat, and liver cells, making it difficult for these cells to absorb glucose from the bloodstream. As a result, the pancreas is prompted to produce more insulin to facilitate glucose absorption, a condition known as hyperinsulinemia.
The Role of Insulin in the Body
- Breakdown of Food into Glucose: When food is consumed, it is broken down into glucose, the primary energy source for the body.
- Release of Insulin: The presence of glucose in the bloodstream triggers the pancreas to release insulin.
- Glucose Uptake: Insulin assists in the uptake of glucose into muscle, fat, and liver cells where it can be utilized for energy or stored for future use.
- Regulation of Blood Glucose Levels: As cells absorb glucose, blood glucose levels decrease, signaling the pancreas to reduce insulin production.
Factors Contributing to Insulin Resistance
Insulin resistance can be influenced by both genetic and lifestyle factors. Key contributors include:
- Obesity: Particularly excess fat around the abdomen and organs, known as visceral fat, which is closely linked to insulin resistance.
- Physical Inactivity: Lack of exercise can exacerbate insulin resistance and its associated conditions.
- Chronic Inflammation: Substances produced by belly fat can lead to persistent inflammation, affecting insulin function.
- Genetic Predisposition: Individuals with a family history of type 2 diabetes are at a higher risk.
Metabolic Implications of Insulin Resistance
Insulin resistance can disrupt normal metabolic functions, leading to several health issues:
- Hyperglycemia: Elevated blood glucose levels due to the cells’ reduced ability to take up glucose.
- Dyslipidemia and Hypertension: Imbalances in blood lipid levels and increased blood pressure.
- Endothelial Dysfunction and Increased Cardiovascular Risk: Poor blood vessel function leading to heightened risk of cardiovascular diseases.
This condition, if unmanaged, may progress to more severe metabolic disorders, including type 2 diabetes and nonalcoholic fatty liver disease (NAFLD). Regular monitoring and management of blood glucose levels are crucial for those at risk of or experiencing insulin resistance.
Causes of Insulin Resistance
Acquired Causes
- Excess Body Fat: Obesity, particularly the accumulation of fat around the abdomen and organs (visceral fat), is a significant risk factor for insulin resistance. This type of fat is not merely inert tissue but actively secretes hormones and other substances that can cause chronic inflammation, a contributing factor to insulin resistance.
- Physical Inactivity: Regular physical activity enhances the body’s sensitivity to insulin and helps in muscle glucose absorption. Conversely, a sedentary lifestyle can lead to increased body fat and decreased muscle mass, both of which contribute to the development of insulin resistance.
- Dietary Factors: High-sodium diets, excessive intake of fructose (often found in processed foods and soft drinks), and overall nutritional imbalances can exacerbate the risk of developing insulin resistance. These dietary habits can lead to an overflow of fat from subcutaneous to visceral stores, promoting insulin resistance.
- Medications: Certain medications, including steroids, blood pressure medications, and some treatments for HIV and psychiatric conditions, have been noted to induce insulin resistance.
Hormonal and Genetic Factors
- Hormonal Disorders:
- Cushing’s Syndrome: Characterized by excessive cortisol, a hormone that increases blood sugar levels and antagonizes insulin’s effects.
- Acromegaly: Elevated growth hormone levels in this condition can lead to increased glucose production and insulin resistance.
- Hypothyroidism: An underactive thyroid slows metabolism, including glucose metabolism, contributing to insulin resistance.
- Genetic Conditions:
- Myotonic Dystrophy and Werner Syndrome: These conditions affect muscle and general metabolic function, leading to significant insulin resistance.
- Lipodystrophy: Affects how the body uses and stores fat, often leading to insulin resistance due to improper glucose storage.
- Polycystic Ovarian Syndrome (PCOS): Commonly associated with insulin resistance, characterized by hormonal imbalances that affect metabolic processes.
Inherited Severe Insulin Resistance Syndromes
These are rare genetic disorders that significantly impair insulin action:
- Type A and Type B Insulin Resistance Syndromes: Both involve severe insulin resistance due to abnormalities at the genetic level affecting insulin receptors or due to autoantibodies against these receptors.
- Rabson-Mendenhall and Donohue Syndromes: These syndromes present early in life with severe insulin resistance and multiple metabolic complications, often leading to early mortality.
Metabolic Processes
Recent studies suggest that insulin resistance may also stem from specific metabolic processes independent of traditional factors like obesity and inactivity. For instance, the activation of carbohydrate-responsive element-binding protein (ChREBP) by fructose consumption has been implicated in the development of insulin resistance by promoting continued glucose production in the liver, despite the action of insulin.
This comprehensive understanding of the causes of insulin resistance highlights the complexity of the condition and underscores the importance of multifaceted approaches in its management.
Symptoms of Insulin Resistance
Identifying Symptoms of Insulin Resistance
Insulin resistance often presents no noticeable symptoms initially, making it a silent condition that can persist undetected for years. Regular medical check-ups that include blood tests are essential as they are the primary method for detecting this condition.
Common Signs and Symptoms
The symptoms associated with insulin resistance are diverse and can vary widely among individuals. Here are some of the most commonly observed signs:
- Increased Waist Circumference:
- Men: Over 40 inches
- Women: Over 35 inches
- Elevated Blood Pressure:
- Readings of 130/80 mmHg or higher
- Abnormal Blood Lipid Levels:
- Fasting glucose level: Over 100 mg/dL
- Fasting triglyceride level: Over 150 mg/dL
- HDL cholesterol level: Under 40 mg/dL in men and 50 mg/dL in women
- Physical Signs:
- Presence of skin tags
- Development of acanthosis nigricans, characterized by dark, velvety skin patches typically found under the arms or on the neck
- Ocular Changes:
- Damage to tiny blood vessels in the eyes leading to retinopathy
Symptoms Indicative of Worsening Condition
If insulin resistance progresses and the pancreas can no longer compensate by increasing insulin production, blood sugar levels may rise, leading to more noticeable symptoms:
- Increased thirst and frequent urination
- Heightened hunger, even after meals
- Blurred vision and headaches
- Recurrent infections, particularly skin and vaginal infections
- Slow-healing cuts and sores
Prediabetes Symptoms
In many cases, insulin resistance advances to prediabetes, where blood sugar levels are high but not yet high enough to qualify as diabetes. Symptoms during this stage can be subtle or non-existent, often going unnoticed for years. However, some individuals might experience:
- Acanthosis nigricans
- Additional skin tags
- Early signs of diabetes-related retinopathy
Understanding and recognizing these signs and symptoms can play a crucial role in early detection and management of insulin resistance, preventing its progression to more severe health issues like type 2 diabetes. Regular monitoring of one’s health with professional medical advice is recommended to manage and potentially mitigate the risks associated with insulin resistance.
Diagnosis of Insulin Resistance
Overview of Diagnostic Tests
Diagnosing insulin resistance involves a variety of tests, as there isn’t a single test that can directly diagnose the condition. Healthcare providers consider several factors, including medical and family history, physical exams, and specific test results.
Commonly Used Tests
- Fasting Plasma Glucose (FPG) Test: This test measures blood sugar levels after an overnight fast. It is one of the primary tests used to screen for prediabetes and diabetes.
- Oral Glucose Tolerance Test (OGTT): After fasting, a person consumes a glucose-containing drink, and blood sugar levels are measured over the next two hours. This test is sensitive and can detect diabetes and prediabetes earlier than the FPG.
- Hemoglobin A1c Test: Reflects average blood glucose levels over the past three months. It is used widely for diagnosing type 2 diabetes and prediabetes but may miss some cases that the OGTT would detect.
Advanced Diagnostic Tools
- Fasting Insulin Assessment: Measures insulin levels after an overnight fast. High levels may indicate insulin resistance.
- Glucose Tolerance Testing (GTT): Detailed glucose tolerance tests can show how the body handles glucose post-meal and are crucial for diagnosing gestational diabetes.
- Modified Insulin Suppression Test: This test involves administering medications to suppress and then stimulate insulin production while measuring blood sugar responses.
Indicators of Prediabetes
| Test | Prediabetes Range |
|---|---|
| A1C | 5.7% to 6.4% |
| Fasting Plasma Glucose | 100 to 125 mg/dL |
| Oral Glucose Tolerance | 140 to 199 mg/dL |
Additional Measures
Healthcare providers may also use tests to diagnose conditions associated with insulin resistance, such as metabolic syndrome, cardiovascular disease, and PCOS. These include lipid panels to assess cholesterol levels and other blood lipids linked to insulin resistance.
Through these diagnostic tools, doctors can assess the presence and extent of insulin resistance, guiding potential treatment options and management strategies to mitigate the risk of developing type 2 diabetes and other associated conditions.
How Insulin Resistance Leads to Diabetes
Insulin resistance marks a critical step in the development of type 2 diabetes, a condition that affects millions worldwide. It typically precedes the onset of diabetes by 10 to 15 years and is characterized by the body’s diminished ability to respond to insulin effectively. This resistance primarily impacts insulin-dependent tissues such as skeletal muscle, which is crucial for glucose disposal.
The Cycle of Insulin Resistance and Hyperinsulinemia
- Initial Response and Compensation: In the early stages, as the body’s cells become resistant to insulin, the pancreas compensates by producing more insulin. This state is known as hyperinsulinemia.
- Increased Demand on Pancreas: Over time, the continuous need for higher insulin levels places excessive strain on the pancreatic beta cells.
- Beta-cell Fatigue: Eventually, these cells fail to keep up with the body’s insulin demands, leading to insufficient insulin production relative to the glucose present in the blood.
Progression to Type 2 Diabetes
- Chronic Hyperglycemia: As the pancreatic function declines, it results in persistent high blood sugar levels, a hallmark of type 2 diabetes.
- Metabolic Changes: The body’s inability to manage glucose effectively leads to various metabolic disruptions, further exacerbating insulin resistance and the risk of developing diabetes.
Impact of Lifestyle Factors
Weight gain and dietary habits play significant roles in the progression from insulin resistance to diabetes. Excessive calorie intake, particularly in the form of simple sugars and fats, can accelerate the onset of hyperinsulinemia and subsequent insulin resistance. While weight gain is commonly observed alongside hyperinsulinemia, it is often the result of chronic caloric excess rather than the insulin levels themselves.
Genetic and Environmental Influences
Both genetic predisposition and lifestyle factors such as physical inactivity and poor diet contribute to the development of insulin resistance. Individuals with a family history of type 2 diabetes are particularly susceptible. Environmental factors, including stress and lack of sleep, can also exacerbate insulin resistance, pushing the individual closer to developing diabetes.
Understanding these mechanisms is crucial for early intervention and management, potentially delaying or preventing the onset of type 2 diabetes. Regular exercise, a balanced diet, and maintaining a healthy weight are key strategies in managing insulin sensitivity and reducing the risk of diabetes.
Treatment and Management of Insulin Resistance
Lifestyle Modifications
The cornerstone of managing insulin resistance effectively involves comprehensive lifestyle modifications. These changes not only help in managing insulin resistance but also contribute to overall health improvement.
- Healthy Diet:
- Limit intake of carbohydrates that stimulate excess insulin production.
- Reduce consumption of unhealthy fats, sugars, red meats, and processed starches.
- Focus on a diet rich in vegetables, fruits, whole grains, fish, and lean poultry.
- Regular Physical Activity:
- Engage in moderate-intensity physical activities regularly.
- Activities such as brisk walking, cycling, or swimming can significantly enhance muscle insulin sensitivity.
- A single session of moderate-intensity exercise can boost glucose uptake by at least 40%.
- Weight Management:
- Aim to lose excess weight to improve insulin sensitivity.
- A reduction of 7% in excess weight can decrease the risk of developing type 2 diabetes by 58%.
Medication and Additional Healthcare Support
While no medications currently target insulin resistance directly, several can be prescribed to manage coexisting conditions:
- Blood Pressure Medications: Helps in managing hypertension which often coexists with insulin resistance.
- Statins: Prescribed to lower LDL (“bad”) cholesterol levels.
Patients are often advised to work closely with a team of healthcare providers, including nutritionists and endocrinologists, to tailor an individualized treatment plan.
Managing Stress and Sleep
Stress management and adequate sleep are crucial in managing insulin resistance effectively:
- Stress Management: High stress levels can spike blood sugar levels, so managing stress through techniques like mindfulness, yoga, or professional counseling is beneficial.
- Adequate Sleep: Less than seven hours of sleep per night can increase insulin resistance. Avoiding naps post-3 p.m. and reducing alcohol and large meals before bedtime can help improve sleep quality.
Smoking Cessation and Dietary Choices
- Avoid Smoking: Tobacco use can exacerbate insulin resistance, so cessation is strongly recommended.
- Dietary Adjustments:
- Increase intake of high-fiber foods which help in managing blood sugar levels by keeping you satiated longer.
- Opt for low-glycemic foods that do not spike your blood sugar rapidly.
Recommended Diets
Two diets that may benefit individuals with insulin resistance include:
- DASH Diet: Known for its potential to reduce hypertension, this diet can also lessen insulin resistance and aid in weight management.
- Mediterranean Diet: Emphasizes healthy fats, fruits, vegetables, and whole grains, and has been shown to help with insulin resistance.
Supplements
While more research is needed, certain supplements might help manage blood sugar levels:
- Cassia Cinnamon
- Ginseng
- Magnesium
Always consult with a healthcare provider before starting any supplements to ensure they are safe and appropriate for your health needs.
Conclusion
Throughout this comprehensive exploration of insulin resistance, we’ve uncovered the complexity of its causes, symptoms, diagnostics, and the pivotal role it plays in the progression to type 2 diabetes. From understanding the intricate balance of insulin’s function in the body to recognizing the interplay of genetic, lifestyle, and environmental factors, the importance of early detection and management becomes increasingly clear. This knowledge equips us to adopt proactive measures in addressing insulin resistance, potentially staving off its progression to more severe metabolic conditions.
Emphasizing lifestyle modifications, such as improved diet, regular physical activity, and weight management, alongside medical interventions, can significantly influence one’s quality of life and overall health prognosis. By embracing these changes and understanding the personal and broader implications of insulin resistance, individuals can make informed decisions toward healthier lifestyles. Furthermore, the encouragement of further research and dialogue in this area promises to unveil more about insulin resistance, offering hope for more effective treatments and management strategies in the future.