Uterine fibroids are a common concern for many women, affecting their health and quality of life. These noncancerous growths in the uterus can cause a range of symptoms, from heavy menstrual bleeding to pelvic pain. Despite their prevalence, many women remain unaware of the impact these growths can have on their reproductive health and overall well-being.
This article aims to shed light on uterine fibroids, exploring their identification, causes, and treatment strategies. We’ll dive into the clinical presentation and diagnosis of these growths, helping readers understand the signs to watch for. Additionally, we’ll discuss various management and treatment options available, providing valuable insights for those affected by or interested in learning more about this condition.
Uterine Fibroids: An Overview
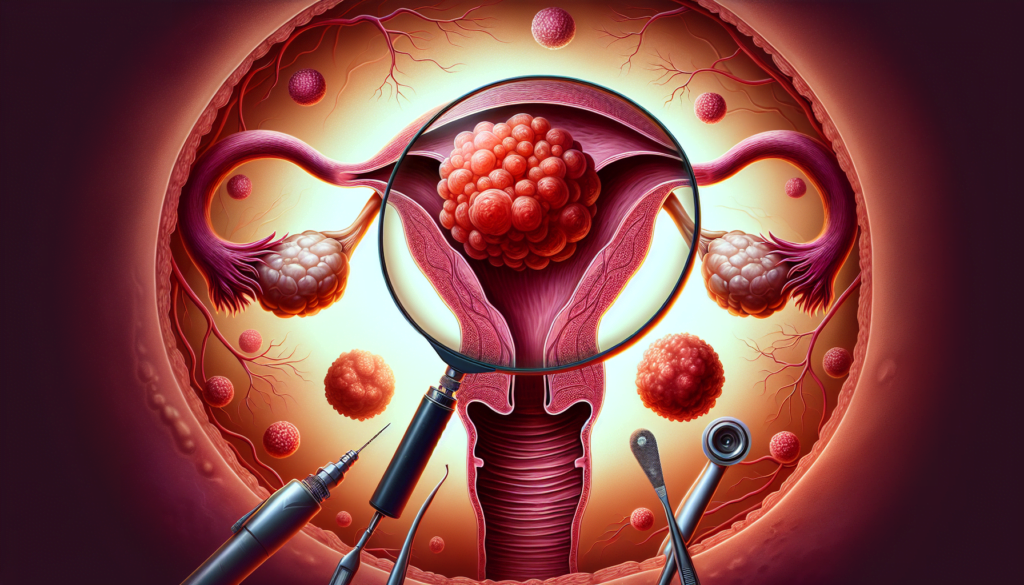
Uterine fibroids, also known as leiomyomas, are noncancerous growths that develop within the muscular wall of the uterus. They are composed of smooth muscle cells and fibrous connective tissue. Fibroids can vary in size, ranging from small seedlings to large masses that distort the shape of the uterus. The location of these growths also varies, with some developing within the uterine wall (intramural fibroids), others protruding into the uterine cavity (submucosal fibroids), and some extending outward from the uterine surface (subserosal fibroids).
The exact cause of uterine fibroids remains unknown, but several factors are believed to influence their development. Hormones, particularly estrogen and progesterone, play a significant role in fibroid growth. Fibroids tend to grow during reproductive years when hormone levels are high and shrink after menopause when hormone levels decline. Genetic factors may also contribute to fibroid development, as women with a family history of fibroids are more likely to develop them.
RELATED: Effective Malaria Treatments and Prevention Methods
Uterine fibroids are remarkably common, affecting a significant portion of the female population. Estimates suggest that 40% to 80% of women will develop fibroids at some point in their lives. The prevalence of fibroids increases with age, peaking during the late reproductive years. African American women are more likely to develop fibroids and tend to experience them at a younger age compared to other racial groups.
Several risk factors have been identified for the development of uterine fibroids. In addition to age and race, other factors include obesity, early onset of menstruation, nulliparity (having never given birth), and a diet high in red meat and low in green vegetables. While these factors may increase the likelihood of developing fibroids, their presence does not guarantee fibroid formation.
The clinical presentation of uterine fibroids varies widely, with some women experiencing no symptoms while others suffer from significant discomfort. Common symptoms include heavy or prolonged menstrual bleeding, pelvic pain or pressure, frequent urination, constipation, and pain during intercourse. In rare cases, fibroids can interfere with fertility or cause complications during pregnancy.
Diagnosis of uterine fibroids typically involves a combination of physical examination, imaging studies, and sometimes, hysteroscopy. Pelvic ultrasound is the most common imaging modality used to visualize fibroids, while MRI provides more detailed information about their size, location, and number. Hysteroscopy allows direct visualization of the uterine cavity and can help identify submucosal fibroids.
Treatment options for uterine fibroids depend on the severity of symptoms, the size and location of the fibroids, and the patient’s desire for future fertility. Medical management may include hormonal therapies, such as oral contraceptives to control symptoms. Surgical options range from minimally invasive procedures, such as hysteroscopic resection or uterine artery embolization, to more extensive surgeries, such as myomectomy or hysterectomy.
In conclusion, uterine fibroids are a common gynecological condition that can significantly impact a woman’s quality of life. Understanding the epidemiology, risk factors, and clinical presentation of fibroids is crucial for timely diagnosis and appropriate management. With advancements in medical and surgical treatments, women with symptomatic fibroids have a range of options to alleviate their symptoms and improve their overall well-being.
Clinical Presentation and Diagnosis
The clinical presentation of uterine fibroids varies widely, with some women experiencing no symptoms while others suffer from significant discomfort. Common symptoms include heavy or prolonged menstrual bleeding, pelvic pain or pressure, frequent urination, constipation, and pain during intercourse. In rare cases, fibroids can interfere with fertility or cause complications during pregnancy.
Symptom Spectrum
The most common symptom of uterine fibroids is abnormal uterine bleeding, usually excessive menstrual bleeding. Other symptoms may include:
- Pelvic pressure or pain
- Frequent urination
- Constipation
- Backache or leg pains
- Pain during intercourse
- Chronic vaginal discharge
The severity of symptoms depends on the size, number, and location of the fibroids. Subserosal fibroids, which grow on the outer surface of the uterus, may cause pelvic pressure or pain. Submucosal fibroids, which protrude into the uterine cavity, often cause heavy menstrual bleeding and prolonged periods. Intramural fibroids, embedded in the muscular wall of the uterus, may cause a combination of symptoms.
RELATED: Mononucleosis Symptoms and Treatment: What You Need to Know
Diagnostic Imaging and Tests
Diagnosis of uterine fibroids typically involves a combination of physical examination, imaging studies, and sometimes, hysteroscopy. The most common imaging modalities used to visualize fibroids are:
- Pelvic ultrasound: The preferred initial imaging modality, it can detect the presence, size, and location of fibroids with a sensitivity of 90-99%.
- Magnetic Resonance Imaging (MRI): Provides more detailed information about the size, number, and location of fibroids, as well as helps distinguish between fibroids and other uterine tumors.
- Hysteroscopy: Allows direct visualization of the uterine cavity and can help identify submucosal fibroids. It is particularly useful when planning surgical intervention.
Other diagnostic tests may include:
- Hysterosalpingography (HSG): An X-ray procedure that provides images of the uterine cavity and fallopian tubes after injection of a contrast material.
- Sonohysterography: A specialized ultrasound procedure that involves injecting sterile saline into the uterus to enhance visualization of the uterine cavity.
In some cases, laparoscopy may be performed to evaluate the external surface of the uterus and other pelvic organs. This is especially helpful when differentiating between fibroids and other uterine masses, such as adenomyosis or uterine cancer.
Management and Treatment Options
The management and treatment of uterine fibroids depend on several factors, including the severity of symptoms, the size and location of the fibroids, and the patient’s desire for future fertility. Conservative approaches, pharmacological interventions, and surgical solutions are available to address the diverse needs of women with fibroids.
Conservative approaches include over-the-counter pain medications, such as ibuprofen or naproxen, to alleviate mild pain and reduce heavy menstrual bleeding. Iron supplements may be recommended to replenish the body’s supply of red blood cells in cases of anemia caused by heavy bleeding. Hormonal birth control pills or intrauterine devices (IUDs) can help control heavy bleeding and painful periods, although they may cause fibroids to grow larger in some cases.
RELATED: Listeriosis: Comprehensive Guide to Symptoms and Treatment
Pharmacological interventions target the hormonal factors that influence fibroid growth. Antagonists decrease estrogen and progesterone levels, causing fibroids to shrink and reducing uterine bleeding. These medications may be used to shrink fibroids prior to surgery or to treat anemia. Progestins, synthetic versions of progesterone, thin the uterine lining and may reduce heavy menstrual bleeding. Antihormonal agents or hormone modulators can slow or stop fibroid growth and improve symptoms.
Surgical solutions are considered when conservative approaches and pharmacological interventions fail to provide adequate relief or when fibroids cause significant complications. Myomectomy, the surgical removal of fibroids while preserving the uterus, may be performed using hysteroscopy, laparoscopy, laparotomy, or robotic-assisted techniques. Hysterectomy, the surgical removal of the uterus, is a definitive treatment for fibroids and is best suited for women who do not wish to become pregnant in the future. Minimally invasive surgical approaches, such as laparoscopic or robotic-assisted hysterectomy, offer smaller incisions, quicker recovery times, and less post-operative pain compared to open surgery.
Conclusion
Uterine fibroids have a significant impact on women’s health, affecting their quality of life and reproductive well-being. This article has explored the identification, causes, and treatment strategies for these common growths, shedding light on their clinical presentation, diagnosis, and management options. By understanding the signs to watch for and the available treatments, women can make informed decisions about their healthcare.
As medical science continues to advance, new and improved methods to manage uterine fibroids are emerging. From conservative approaches to cutting-edge surgical techniques, there’s a wide range of options to address the diverse needs of women with fibroids. This means that women suffering from fibroid-related symptoms can work with their healthcare providers to find the most suitable treatment plan, taking into account their individual circumstances and future fertility desires.