Vulvar intraepithelial neoplasia (VIN) is a precancerous condition that affects the skin of the vulva, the external female genital area. This condition can cause significant discomfort and concern for women, as it has the potential to develop into vulvar cancer if left untreated. Understanding VIN is crucial for early detection and effective management, which can greatly improve outcomes for those affected.
This article aims to shed light on vulvar intraepithelial neoplasia, covering its symptoms, diagnosis, and treatment options. Readers will gain insights into recognizing the signs of VIN, learn about the diagnostic process, and explore the various treatment approaches available. By providing this information, we hope to empower women to seek timely medical attention and make informed decisions about their health.
Understanding Vulvar Intraepithelial Neoplasia (VIN)
Vulvar intraepithelial neoplasia (VIN) is a precancerous condition that affects the skin of the vulva, the external female genital area. It occurs when there are changes in the cells of the skin covering the vulva. VIN is not cancer; however, if the changes become more severe, cancer of the vulva may develop after many years.
Definition and Types of VIN
VIN can range from mild to severe and is classified into two main types:
- Usual or classical VIN (uVIN): This includes low-grade squamous intraepithelial lesions (LSIL) and high-grade squamous intraepithelial lesions (HSIL). LSIL is usually caused by low-risk types of human papillomavirus (HPV) and often goes away without treatment. HSIL is caused by high-risk types of HPV and has a risk of developing into cancer over time if left untreated.
- Differentiated VIN (dVIN): This less common type of VIN usually develops in older women and is not linked to HPV infection. It is commonly found in women with a vulval condition called lichen sclerosis and has a higher risk of developing into cancer than HSIL.
RELATED: Atelophobia(Fear of Imperfection): Causes, Symptoms, and How to Overcome It
Risk Factors and Causes
The exact cause of VIN is not known; however, it has been linked to several factors:
- Infection with the human papillomavirus (HPV)
- Smoking
- Having problems with the immune system, such as HIV
- Long-term skin problems, such as lichen sclerosis
Having one or more of these risk factors does not mean an individual will definitely develop VIN.
Prevalence and Demographics
VIN is rare, with an incidence of 2.99 per 100,000 woman-years. The incidence of VIN has been rising over time, with a 38.2% increase between 1991-1995 and 2006-2011. This rising incidence may be due to an aging population, increased burden of HPV-related disease, and greater public and clinical awareness leading to more vulvar biopsies.
VIN is more common in White women than non-White women, with the highest reported incidence occurring during the fourth decade of life. Usual or classical VIN is more common in younger women (average age at presentation, 40 years), whereas differentiated VIN is more common in older women (average age at presentation, 60 years).
Recognizing VIN Symptoms
The symptoms of vulvar intraepithelial neoplasia (VIN) can vary from person to person, and in some cases, there may be no noticeable symptoms at all. However, it is crucial to be aware of the common signs and symptoms of VIN to ensure early detection and prompt treatment.
Common Signs and Symptoms
Some of the most frequently reported symptoms of VIN include:
- Chronic vulvar itching
- Burning, tingling, or soreness in the vulva area
- Pain during sexual intercourse or masturbation
- Changes in the appearance of the affected area, such as redness or discolored skin
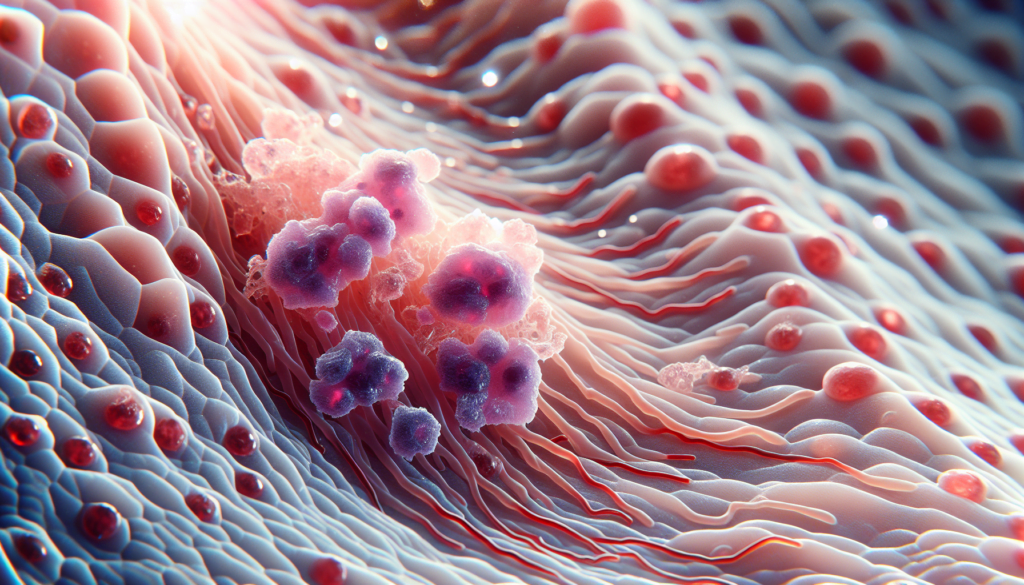
Visual Appearance of VIN Lesions
VIN lesions can manifest in various ways, depending on the type of VIN. Usual VIN (uVIN) typically involves raised lesions, although flat lesions are also possible. These lesions often affect the labia majora and the area around the vaginal opening. On the other hand, differentiated VIN (dVIN) lesions usually appear as patches of thick or discolored skin.
VIN-related bumps may be raised or flat, and they can be a different color than the surrounding skin, resembling moles or freckles. These bumps may change in size, shape, border, or color over time. Additionally, VIN can cause discoloration, with patches of skin appearing white, gray, red, brown, or black. These patches may have a different texture compared to the surrounding area.
RELATED: Articulation Disorder: Symptoms, Diagnosis, and Therapy Options
When to Seek Medical Attention
If you experience any of the above symptoms or notice any suspicious changes in the appearance of your vulva, it is essential to consult a healthcare professional promptly. Even if the symptoms are not caused by VIN, they may indicate another condition that requires treatment.
Regular check-ups and early treatment can help prevent VIN from developing into cancer. Healthcare professionals can accurately diagnose VIN through a physical examination, colposcopy, and biopsy of the affected area. Remember, early detection and intervention are key to maintaining optimal vulvar health.
Diagnosis and Evaluation of VIN
The diagnosis of vulvar intraepithelial neoplasia (VIN) involves a comprehensive clinical examination, biopsy, and histopathological evaluation. Early detection and accurate diagnosis are crucial for appropriate management and prevention of progression to invasive vulvar cancer.
Clinical Examination
A thorough visual inspection of the vulva is the first step in diagnosing VIN. The lesions may appear as raised, flat, white, gray, or pigmented areas on the vulvar skin. They can be single or multifocal, and their appearance may vary. Regular check-ups and early treatment can help prevent VIN from developing into cancer.
During the examination, healthcare professionals assess the location, number, size, shape, color, and thickness of the lesions. A colposcopic examination or a hand lens with magnification may be used to complement the visual exam. If high-grade lesions are discovered, an examination and cytology of the anal canal may also be necessary, as up to 18% of patients with vulvar HSIL may have anal lesions.
Biopsy and Histopathology
Any observed vulvar lesions require a biopsy to confirm the diagnosis and determine the appropriate treatment. The biopsy site is selected based on the most clinically and dermoscopically significant areas. The histological feature necessary for diagnosing VIN is the proliferation of atypical basal cells, which is assessed based on five criteria:
- Basal layer involvement
- Enlarged nuclei
- Hyperchromasia
- Pleomorphic cells
- Increased numbers of mitotic figures
Immunohistochemistry markers, such as p53 and p16, can be used to differentiate between uVIN and dVIN. P53 positivity and p16 negativity support a dVIN diagnosis, whereas the converse supports a uVIN diagnosis.
Differential Diagnosis
The differential diagnosis of VIN includes various benign and malignant conditions, such as:
- Lichen simplex, lichen sclerosis, or lichen planus
- Infections (vestibulitis, candidiasis, or herpes)
- Genital warts, psoriasis, condyloma acuminata, and seborrheic keratosis
- Basal cell carcinoma, squamous cell carcinoma, Paget’s disease, or melanoma
Treatment without biopsy confirmation risks progression and delays the diagnosis of potential malignancy. Therefore, a biopsy is essential for accurate diagnosis and appropriate management of VIN.
Treatment Options for VIN
Treatment options for vulvar intraepithelial neoplasia (VIN) include surgical interventions, topical treatments, laser therapy, and other approaches. The goal of treatment is to remove the abnormal tissue while preserving vulvar function and minimizing morbidity.
Surgical Interventions
Surgical excision is the standard treatment for high-grade VIN lesions. Wide local excision involves removing the lesion with a margin of normal tissue. This approach allows for histological examination of the excised tissue to rule out invasive disease. Loop electrosurgical excision procedure (LEEP) and laser excision are alternative surgical techniques that may be used in select cases.
RELATED: What is Arthus Reaction? Symptoms, Causes, and Treatment Options
Laser Therapy and Other Approaches
Laser ablation, using a CO2 laser, can be an alternative to surgical excision in some cases. This technique preserves normal vulvar anatomy but does not provide a specimen for histological examination. Photodynamic therapy, which involves the use of a photosensitizer and non-thermal light to induce cellular death, has also been investigated as a treatment option for VIN.
The choice of treatment depends on factors such as lesion size, location, and patient preferences. Close follow-up is essential after any treatment modality due to the high risk of recurrence. HPV vaccination may play a role in preventing VIN, but it is not currently used as a treatment for established lesions.
Conclusion
Vulvar intraepithelial neoplasia is a complex condition that has a significant impact on women’s health. This article has shed light on its symptoms, diagnosis, and treatment options, providing crucial information to help women recognize potential signs and seek timely medical attention. Understanding VIN and its management is key to prevent its progression into more serious conditions.
Early detection and proper treatment of VIN are vital to maintain vulvar health and overall well-being. While the condition can be challenging to deal with, various treatment approaches offer hope for effective management. Regular check-ups, awareness of one’s body, and open communication with healthcare providers are essential steps to tackle VIN and ensure optimal outcomes for those affected.