Dry socket, a painful condition that can occur after tooth extraction, is a concern for many dental patients. This complication arises when the blood clot that normally forms in the socket after extraction is dislodged or dissolves, leaving the underlying bone and nerves exposed. Understanding dry socket is crucial for anyone undergoing a tooth extraction, as it can lead to severe discomfort and delayed healing.
This article aims to shed light on the key aspects of dry socket. It will explore the definition and causes of this condition, help readers identify its symptoms, and discuss effective treatment options. Additionally, it will provide valuable tips to prevent dry socket, empowering patients to take an active role in their post-extraction care. By the end, readers will have a comprehensive understanding of this dental complication and how to deal with it.
What is Dry Socket?
Dry socket, also known as alveolar osteitis, is a painful dental condition that can occur after a tooth extraction. It happens when the blood clot that normally forms in the socket to protect the bone and nerves either fails to develop or becomes dislodged before the wound has healed. This exposes the underlying bone and nerves, leading to intense pain and discomfort.
Definition
Dry socket is characterized by severe pain in and around the extraction site, which typically begins one to three days after the procedure. The socket may appear empty, with exposed bone visible. Patients may also experience bad breath or an unpleasant taste in their mouth.
RELATED: What Is Atrial Tachycardia? Symptoms, Causes, and Treatments
Pathophysiology
The exact cause of dry socket is not fully understood, but it is believed to involve a combination of factors. One theory suggests that bacterial contamination of the socket may lead to the premature breakdown of the blood clot. Another theory proposes that trauma during the extraction process or excessive smoking after the procedure may disrupt the formation of the blood clot.
Incidence Rates
The incidence of dry socket varies, but it is estimated to occur in approximately 1-5% of all tooth extractions. However, the risk is significantly higher for certain types of extractions, such as those involving impacted wisdom teeth. In these cases, the incidence rate can be as high as 30%. Factors that may increase the risk of developing dry socket include smoking, oral contraceptive use, poor oral hygiene, and a history of previous dry socket.
Recognizing Dry Socket Symptoms
Dry socket, a painful complication that can occur after tooth extraction, has distinct symptoms that set it apart from normal post-extraction healing. Recognizing these symptoms is crucial for seeking timely treatment and alleviating discomfort.
Pain Characteristics: The primary symptom of dry socket is severe pain that develops within a few days after tooth removal. Unlike normal post-extraction pain, which gradually improves, dry socket pain intensifies over time. The pain may throb and radiate from the extraction site to the ear, eye, temple, or neck on the same side of the face. This pain can be more intense than the discomfort experienced during the extraction procedure itself.
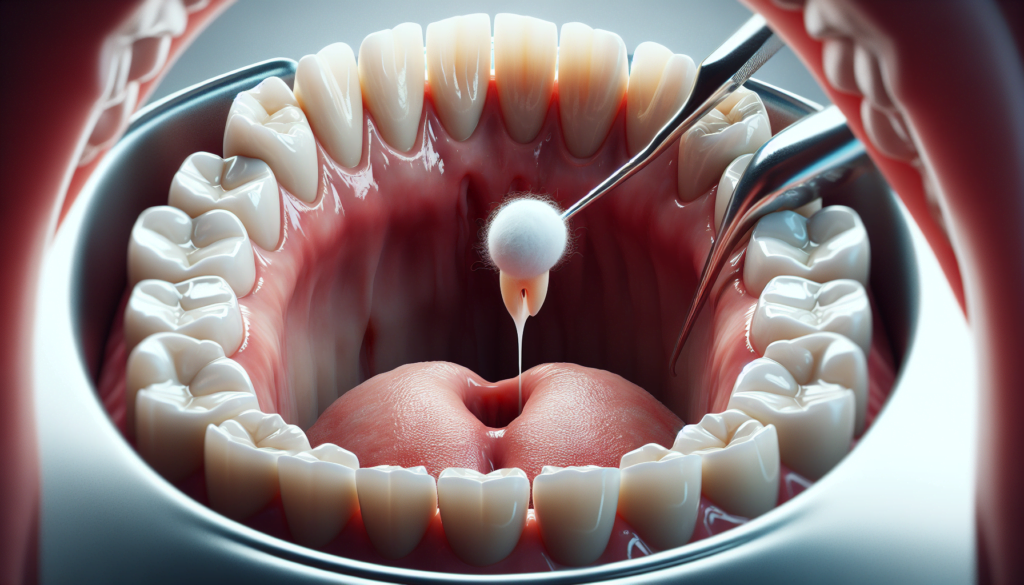
Visual Signs: Visual inspection of the extraction site can reveal telltale signs of dry socket. In a normal healing socket, a blood clot forms to protect the underlying bone and nerve endings. However, in dry socket, this blood clot is either partially or completely absent, exposing the bone. The socket may appear empty, with visible bone tissue. Over time, the exposed bone and tissue may become more apparent as the socket fails to heal properly.
RELATED: Atrial Septal Defect: Symptoms, Diagnosis, and Treatment Explained
Associated Symptoms: In addition to pain and visual changes, dry socket can cause other unpleasant symptoms. Patients may experience a foul odor or bad breath emanating from the mouth, indicating an accumulation of bacteria in the exposed socket. An unpleasant taste in the mouth is another common complaint. The extraction site may also become swollen and irritated, with bits of food debris collecting in the socket and exacerbating the pain.
If you experience any of these symptoms after a tooth extraction, it is essential to contact your dentist or oral surgeon promptly. They can diagnose dry socket and provide appropriate treatment to manage pain and promote proper healing. Early intervention can help alleviate discomfort and prevent further complications.
Medical Intervention for Dry Socket
When a patient presents with symptoms of dry socket, the dentist or oral surgeon will conduct an initial assessment to confirm the diagnosis. This involves examining the extraction site for exposed bone, evaluating the severity of pain, and ruling out other potential causes of discomfort, such as infection or remaining tooth fragments.
Once dry socket has been diagnosed, the primary goal of treatment is to alleviate pain and promote healing. The following procedures are commonly employed:
- Irrigation and Debridement: The extraction socket is gently flushed with saline or chlorhexidine solution to remove any debris, necrotic tissue, or bacteria that may impede healing. This process helps to create a clean environment conducive to the formation of a new blood clot.
- Medicated Dressings: After irrigation, the socket is packed with a medicated dressing, such as zinc oxide eugenol paste or iodoform gauze. These dressings contain analgesic and antimicrobial properties that help to reduce pain and prevent infection. The dressing is typically replaced every few days until symptoms subside.
- Pain Management: Patients are prescribed over-the-counter or prescription pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids, to manage discomfort. Topical anesthetics may also be applied directly to the affected area for immediate relief.
- Antibiotics: In some cases, antibiotics may be prescribed to prevent or treat secondary infections, particularly if the patient is immunocompromised or has a history of systemic conditions that increase the risk of infection.
Follow-up care is essential to ensure proper healing and to monitor for any complications. Patients are advised to maintain good oral hygiene, gently rinsing with warm salt water, and avoiding smoking or using straws, which can dislodge the newly formed blood clot. Regular check-ups with the dentist or oral surgeon are scheduled to assess the progress of healing and to make any necessary adjustments to the treatment plan.
Preventing Dry Socket
Preventing dry socket is crucial to ensure proper healing after tooth extraction. By taking appropriate measures before and after the procedure, as well as making necessary lifestyle changes, patients can significantly reduce their risk of developing this painful condition.
Pre-Extraction Measures
Prior to tooth extraction, it is essential to inform the dentist about any medications or supplements being taken, as some may interfere with blood clotting. Patients should also discuss their smoking habits with the dentist, as smoking can greatly increase the likelihood of dry socket. If possible, quitting smoking or using nicotine patches instead of cigarettes before the procedure can help minimize the risk.
RELATED: Atrial Septal Aneurysm: Key Facts and Treatment Options
Post-Extraction Care
Following the extraction, patients should adhere to their dentist’s aftercare instructions carefully. Avoiding vigorous rinsing, spitting, or using straws for the first 24-48 hours is crucial to prevent dislodging the blood clot. Patients should also refrain from smoking and consuming alcohol during this period. Gently rinsing with warm salt water a few times a day can help keep the extraction site clean without disturbing the clot.
Eating soft foods and avoiding crunchy, hard, or sticky foods that may get stuck in the socket is recommended. Patients should also maintain proper oral hygiene by brushing their teeth gently and using any prescribed antibacterial mouthwash as directed.
Lifestyle Factors
In addition to post-extraction care, certain lifestyle factors can influence the development of dry socket. Smoking is a significant risk factor, as the chemicals in tobacco products can delay healing and cause infection. Patients who smoke should make an effort to quit or at least refrain from smoking for several days after the extraction.
Engaging in strenuous physical activity immediately after the procedure can also increase the risk of dry socket, as it may cause the blood clot to become dislodged. Patients should rest and limit their activities for the first 24-48 hours to promote proper healing.
By taking these preventive measures and following their dentist’s instructions closely, patients can greatly reduce their risk of developing dry socket and ensure a smooth recovery after tooth extraction.
Conclusion
Understanding dry socket and its prevention is key to a smoother recovery after tooth extraction. This dental complication can have a big impact on a patient’s comfort and healing process, making it crucial to know its symptoms and treatment options. By following proper post-extraction care and making smart lifestyle choices, patients can greatly lower their chances of developing dry socket.
In the end, knowledge is power when it comes to dental health. Being aware of the risks and taking steps to avoid dry socket can lead to a quicker and less painful recovery. Remember, if you suspect you might have dry socket after an extraction, don’t hesitate to reach out to your dentist. They’re there to help and can provide the care needed to get your healing back on track.